Scroll to:
Microsurgical removal of a cavernous malformation on the midbrain dorsal surface using the supracerebellar infratentorial approach: a clinical case
https://doi.org/10.47093/2218-7332.2025.1210
Abstract
Common surgical approaches to the dorsal midbrain include: the occipital transtentorial, supracerebellar infratentorial, posterior subtemporal, and the tonsilloveal transaqueductal approaches.
Case report. A 38-year-old man presented with mild right-sided weakness and diplopia following an episode of headache and vomiting two weeks prior to admission. A neurological examination revealed mild right-sided weakness, a downward and outward strabismus, a mild left ocular mydriasis and accommodation paralysis alongside alternating syndrome. Magnetic resonance imaging revealed a 20×30×25 mm rupture of the cavernous malformation of the left midbrain peduncle as well as hematomas within the cavernoma. Using the supracerebellar infratentorial approach in a sitting position with minimal incision of dorsal midbrain, the cavernoma was completely resected together with surrounding subacute hematoma. In the early postoperative period, a regression of neurological symptoms was observed.
Discussion. The choice of median suboccipital craniotomy and contralateral supracerebellar infratentorial approach is the preferred route for complete resection of cavernoma of dorsal midbrain surface in order to avoid any postoperative neurological deficit.
Keywords
Abbreviations:
- CM – cavernous malformation
- CT – computed tomography
- MRI – magnetic resonance imaging
Cavernous malformations (CM) or cavernomas of the central nervous system are formations consisting of multiple adjacent cavities of irregular shape (caverns), lined with endothelium and filled with blood.
According to magnetic resonance imaging (MRI) data at the screening stage and several thousand autopsies, CM of the central nervous system is detected in 0.3–0.6% of the population [1][2]. Most often, the first symptoms appear at a young age – on average, at 23 years [3].
Of all CMs of the brain, localization in the brainstem accounts for 19 to 30% [3], of which 14.2–25% occur in the midbrain [4]. In cerebral CMs, the annual frequency of primary hemorrhages is 0.39-1.3%, recurrent – 4.5–22.9% [5]. It is believed that brain cavernomas located in the brainstem area are most prone to recurrent hemorrhages with an annual risk ranging from 21–60% and complications during surgical intervention than with other localizations of cavernomas [6–9]. The risk of recurrent bleeding increases with incomplete surgical resection [9][10]. These features allow to distinguish brainstem CMs into a separate group.
The tactics of surgical treatment of primary bleeding from the midbrain CM depend on the timing of the hemorrhage, age and somatic status of the patient and necessitate an individual approach to developing an optimal treatment strategy.
The purpose of this case report is to demonstrate the experience of successful radical resection of the midbrain peduncle CM by the supracerebellar infratentorial approach as an effective surgical strategy for primary hemorrhage in a young patient.
CASE REPORT
A 38-year-old man, a builder, sought medical help at the SI “National Medical Center of the Republic of Tajikistan Shifobakhsh” on May 13, 2024 with complaints of diplopia and mild weakness in the right limbs, which arose suddenly after an episode of headache and vomiting about two weeks previously.
Clinical examination on admission: clear consciousness, 15 points according to the Glasgow Coma Scale, somatic status without any peculiarities: respiratory rate 16 per minute, heart rate 80 per minute, blood pressure 120/80 mm Hg. In the neurological status, a slight decrease in strength on the right side was noted – IV/V degree according to the classification of muscle tone study1, strabismus downward and outward, mild mydriasis and paralysis of accommodation of the left eye alongside alternating syndrome.
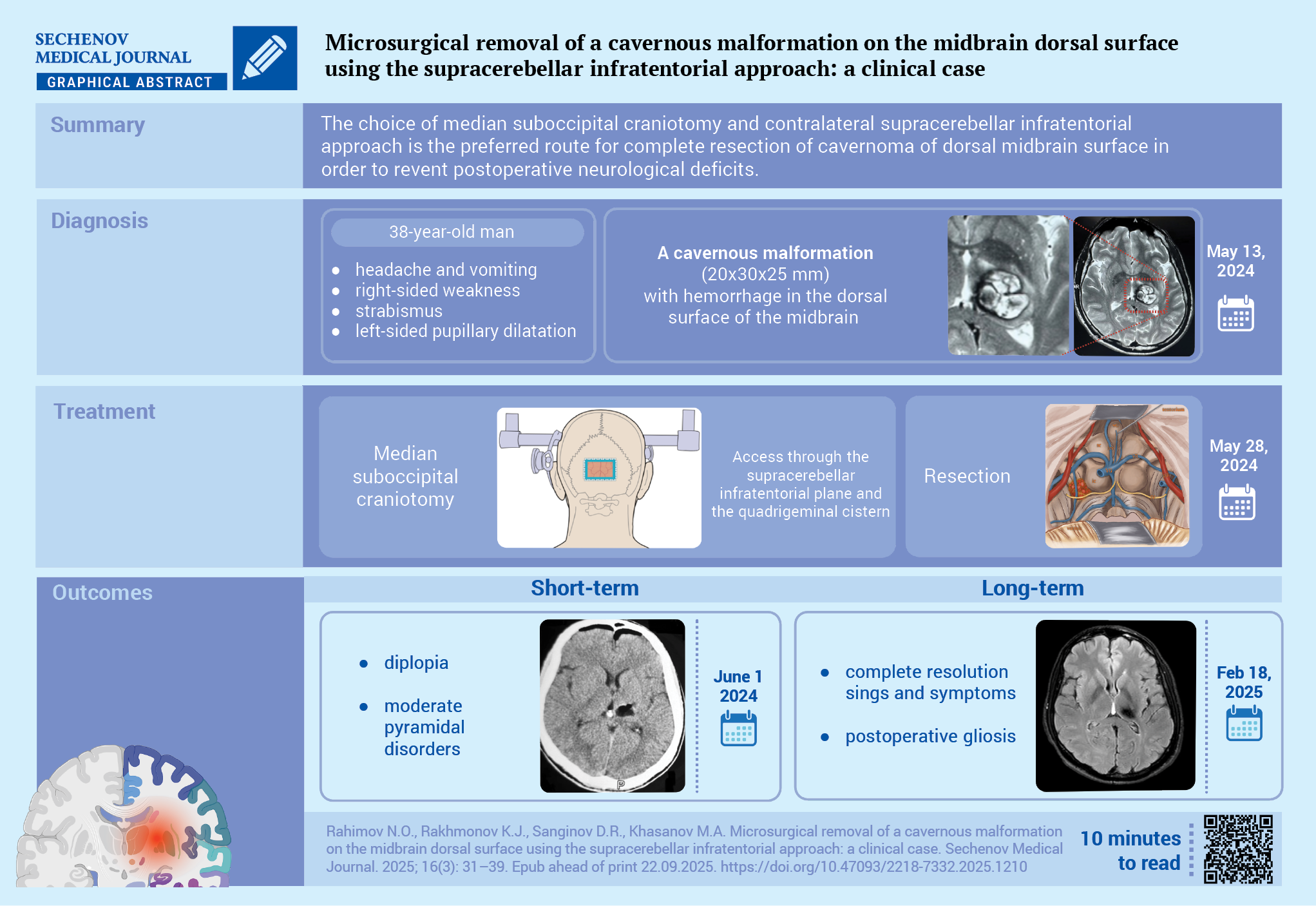
Computed tomography (CT) of the brain revealed a poorly defined hyperdense formation in the lower part of the dorsal surface of the left peduncle of the midbrain measuring 20x30x25 mm. MRI of the brain revealed a hyperintense lesion in T1- and T2-weighted images with a clearly defined hypointense rim, hematomas in a cavernoma of 20×30×25 mm (Fig. 1A–C).
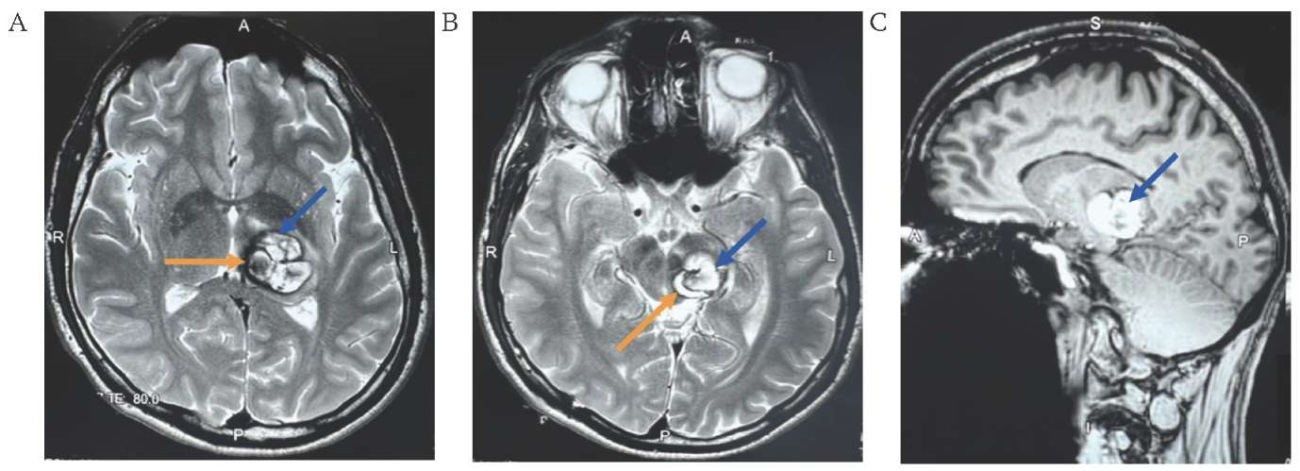
FIG. 1. Magnetic resonance imaging of a 38-year-old patient with a cavernous malformation measuring 20×30×25 mm in the dorsal part of the left peduncle of the midbrain (May 13, 2024).
A, B. Axial sections, T2-weighted image: cavernous malformation (blue arrow), hematomas in the cavernoma (orange arrow).
C. Sagittal section, T1-weighted image: cavernous malformation (arrow).
Based on clinical data and neuroimaging results, the following diagnosis was made: rupture of CM of the left midbrain peduncle, hematomas in the cavernoma.
To avoid any postoperative neurological deficit (as assessed by additional scales: 4 points on the Spetzler–Martin [11] and 3 points on the Lawton–Young [12]), a median suboccipital craniotomy with a contralateral supracerebellar infratentorial approach was chosen for radical cavernoma resection (Fig. 2A–E).
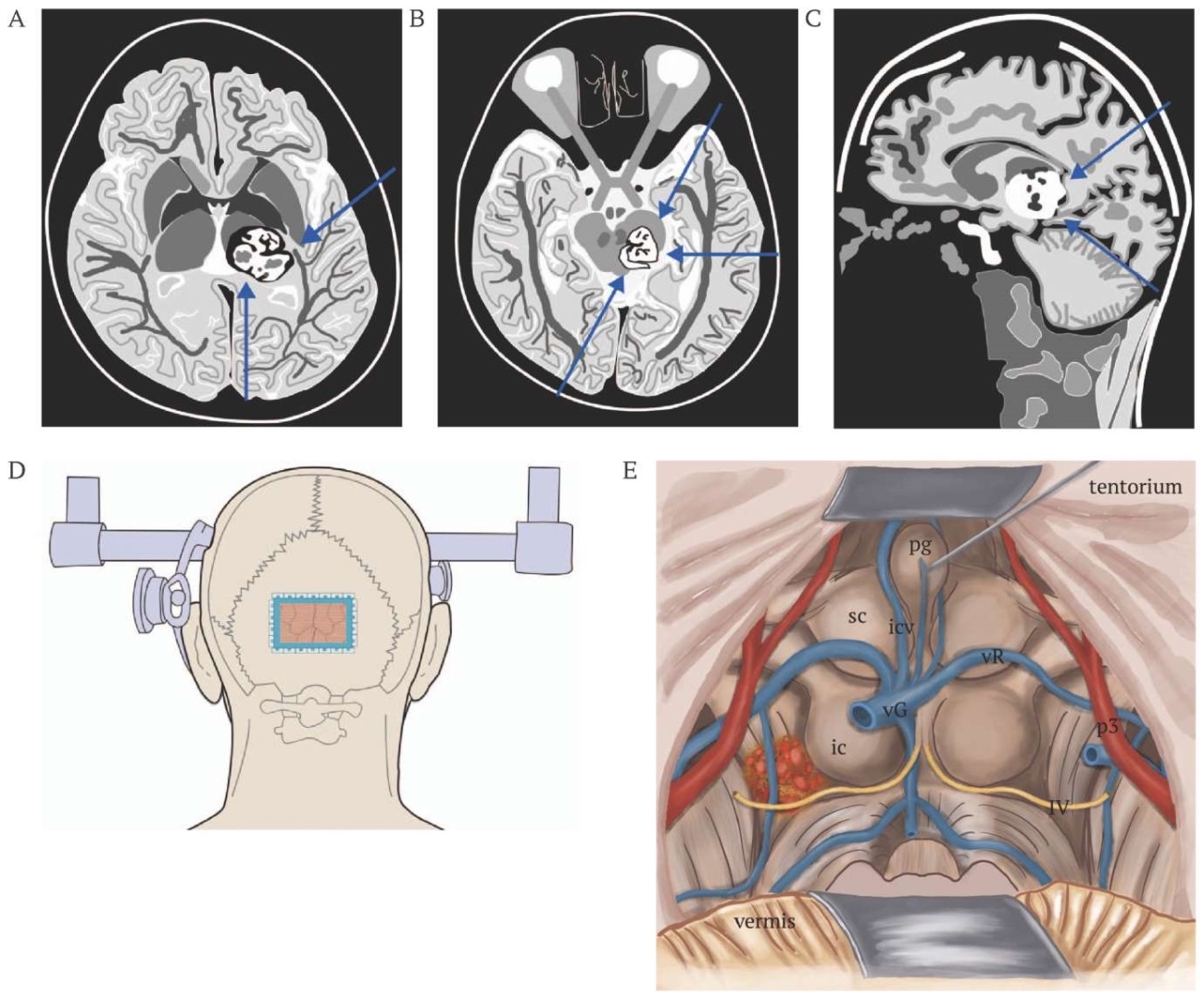
FIG. 2. Schematic representation of the localization of the cavernoma of the dorsal surface of the midbrain and the choice of strategy for its resection.
A. Axial section. The arrows indicate the approaches to the midbrain: left lower – supracerebellar infratentorial; right upper – posterior subtemporal.
B. Axial section. The arrows indicate the approaches to the midbrain: left lower – contralateral supracerebellar infratentorial; right upper – anterior subtemporal; right lower – posterior subtemporal approaches.
C. Sagittal section. The arrows indicate the approaches to the midbrain: right upper – occipital transtentorial; right lower – supracerebellar infratentorial.
D. Exposure of the cavernoma using torcular craniotomy and supracerebellar infratentorial approach (blue line).
E. Access to the cavernoma through the supracerebellar infratentorial plane and the quadrigeminal cistern; identification of the ascending deep cerebral veins; determination of the feeding arteries of the pons and midbrain; review of the lateral sections; dissection of the quadrigeminal cistern to provide a free corridor (superior view of the midbrain, pons, tentorium from the pineal region and superior cerebellar peduncle); mobilization of the vessels and veins draining into the superior sagittal sinus.
Note: ic – inferior colliculus; icv – internal cerebral vein; pg – pineal gland; p3 – posterior cerebral artery (segment p3); sc – superior colliculus; vG – vein of Galen; vR – vein of Rosenthal; IV – cranial nerves (IV pair).
Surgery Procedure
The operation was performed on May 28, 2024 under general endotracheal anesthesia with the patient in a sitting position – to give the back a vertical position, and with the head tilted forward to smooth the angle of the tentorium. The patient’s head was rigidly fixed using a Mayfield-Keys clamp. The Carl Zeiss OPMI Vario S88 operating microscope (Carl Zeiss, Germany) was used during the operation.
Surgical access was achieved through a 12 cm long linear skin incision in the parietal-occipital region. A burr hole was created in the occipital protuberance region, which provided a circular craniotomy measuring 80x60 mm with exposure of the sinus drain and contralateral supracerebellar infratentorial access with gravitational retraction of the cerebellum. The upper edge of the bone flap was located on the transverse sinus.
A semi-oval incision of the dura mater, reinforced with interrupted sutures, was made, which elevated the transverse sinuses and provided entry into the supracerebellar infratentorial plane. The sagging of the cerebellum widened the natural corridor to the quadrigeminal cistern. Cerebrospinal fluid was drained from the cisterna magna, and the cerebellum was retracted by dissection of the arachnoid adhesions connecting the posterior superior border of the cerebellum to the outer edge of the tentorium. To access the free edge of the tentorium, the bridging veins between the cerebellum and the tentorium were divided. The arachnoid membrane dissection of the posterior edge of the quadrigeminal cistern was performed to visualize the dorsal part of the midbrain.
The supracerebellar infratentorial approach in the sitting position opens the anatomical plane so widely that dissection is significantly facilitated. Any discomfort from working with raised arms is compensated by the panorama without a retractor and the operative field cleared by gravity (Fig. 3A). Arachnoid dissection was performed, and large deep veins (V. Galen, internal cerebral veins, internal occipital veins, basal veins of Rosenthal, pericentral veins of the cerebellum) were identified. The contralateral approach allowed visualization of the IV pair of cranial nerves and the P3 segment of the posterior cerebral artery.
With a minimal incision in the dorsal part of the midbrain (Fig. 3B), the cavernoma was completely resected together with the surrounding subacute hematoma measuring 2×3×2.5 cm (Fig. 3C). Hemostasis was achieved until the lavage water was clear. A hemostatic collagen sponge was placed in the cavernoma bed. The dura mater was sutured hermetically. The bone flap was fixed with threads. Layer-by-layer suturing of the wound was performed. An aseptic dressing was applied. The total blood loss was 250 ml.
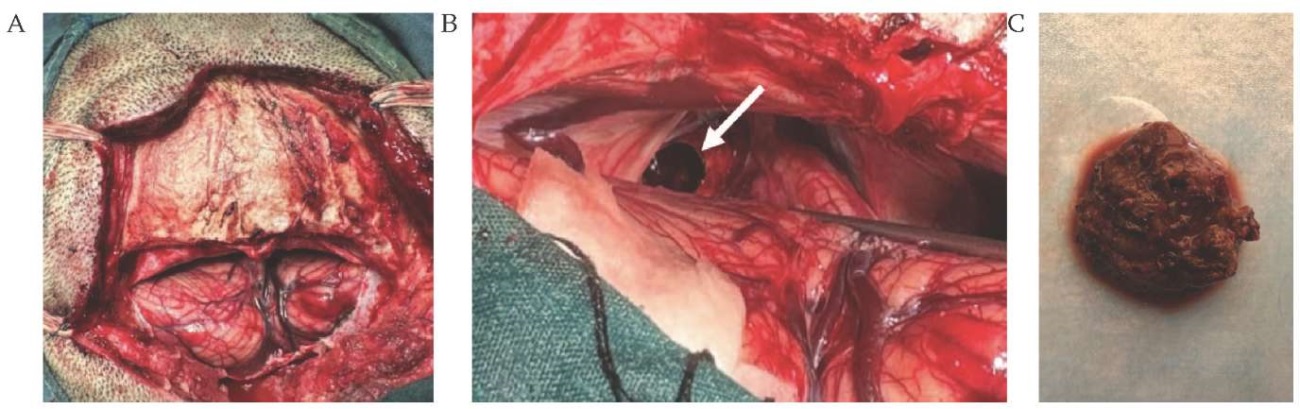
FIG. 3. Resection of the cavernous malformation of the midbrain peduncle via the supracerebellar infratentorial approach in a 38-year-old man (May 28, 2024).
A. General view of the supracerebellar infratentorial approach after opening the dura mater.
B. Incision of the dorsal part of the midbrain, approach to the cavernoma (arrow).
C. Macropreparation of the removed cavernoma 2×3×2.5 cm.
A control CT scan in the postoperative period was performed on the third day; according to the study data, the condition after median suboccipital craniotomy, residual cavernoma, and repeated hemorrhage were not detected (Fig. 4A, B).
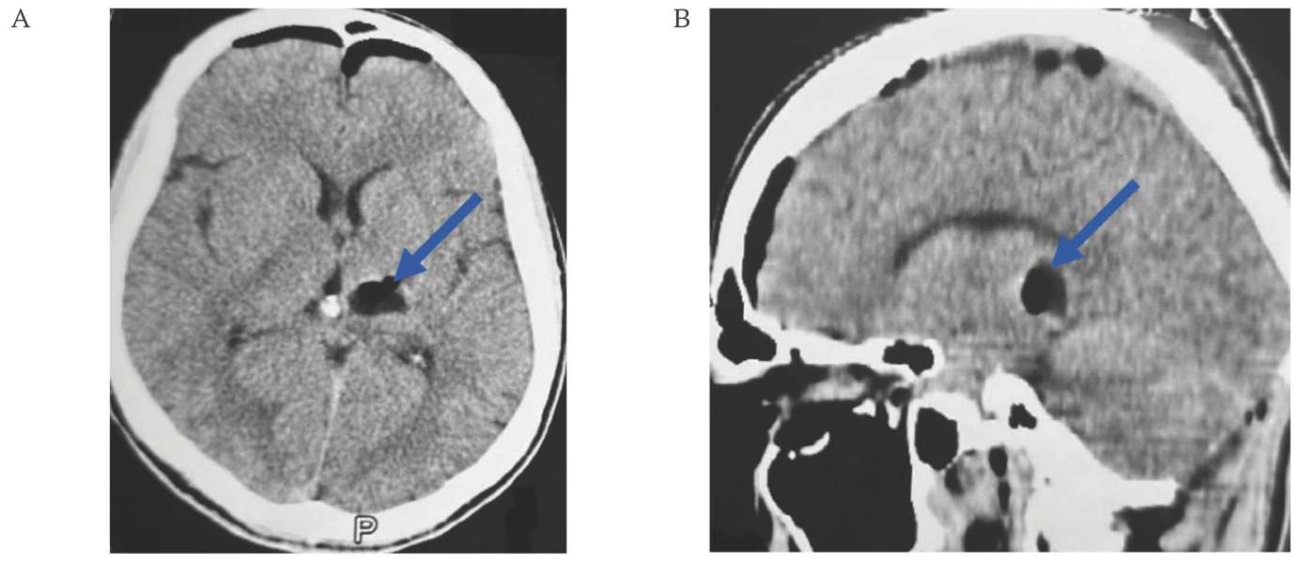
FIG. 4. Computed tomography of a 38-year-old patient on the 4th day after removal of a cavernous malformation in the dorsal part of the left peduncle of the midbrain (June 01, 2024).
A. Axial section: the cavernoma with the hematoma capsule is completely resected (arrow).
B. Sagittal section: the cavernoma with the hematoma capsule is completely resected (arrow).
In the postoperative period, the patient’s consciousness is clear (15 points on the Glasgow Coma Scale), diplopia and moderate pyramidal disorders disappeared on the 12th day. The course of the postoperative period is smooth, without the development of postoperative complications. The patient was discharged from the hospital on the 15th day after the surgical intervention.
The patient came for a follow-up examination and assessment of the long-term treatment results on February 18, 2025. During the examination, the patient’s consciousness was clear. No sensory or motor disturbances were observed after the surgery. He was able to walk and take care of himself independently. The patient has fully recovered and returned to professional activities without any restrictions.
A MRI of the brain was undertaken on February 18, 2025, and here we can observe the brain’s condition after removal of the cavernoma. The MR showed signs of postoperative gliosis changes. No residual cavernoma or recurrent hemorrhage was detected (Fig. 5A, B).
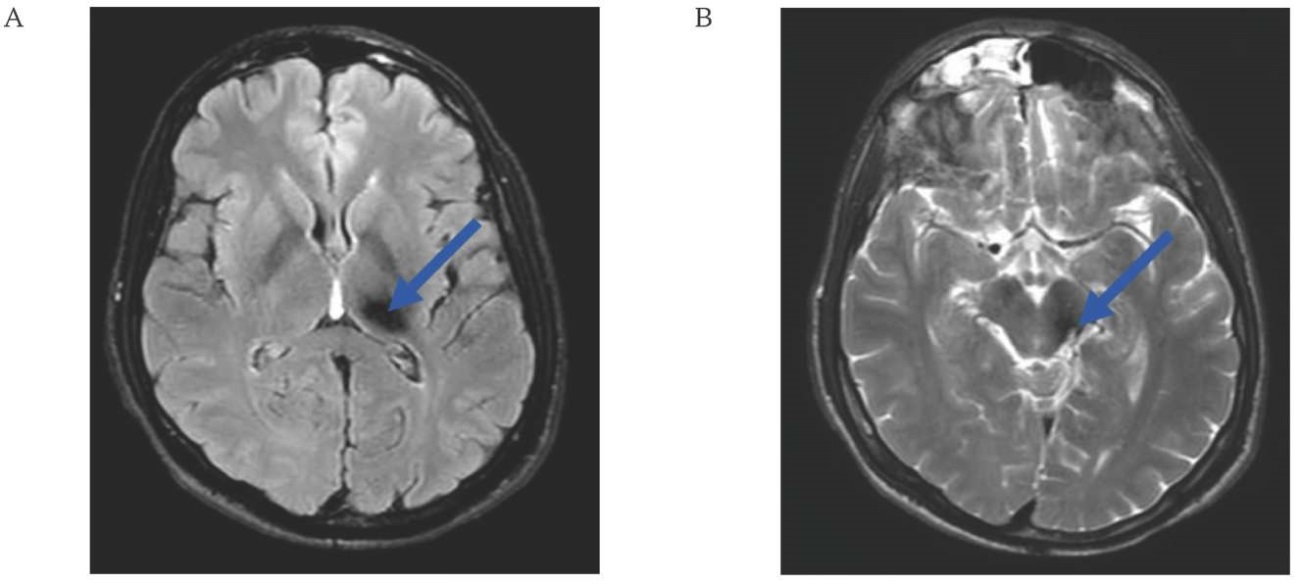
FIG. 5. Magnetic resonance imaging of the brain of a 38-year-old patient 9 months after resection of a cavernous malformation in the dorsal part of the left peduncle of the midbrain (February 18, 2025)
A, B. Axial sections: postoperative gliotic changes (arrows).
DISCUSSION
At present, one of the main issues in treating midbrain CM is determining the timing of the surgical intervention, be it in the acute or the subacute period.
In our case, the patient was operated on the 20th day after the primary hemorrhage. The cavernoma was located in the subacute hematoma, which made it easy to remove together with the cavernoma itself.
According to generally accepted practice and in line with our clinical experience, surgical treatment in the subacute stage of hemorrhage, when the hematoma is liquefied, is effective for maximum removal of the hematoma with minimal incision of the brainstem [13]. In such cases, a limited incision of the brainstem contributes to the most complete neurological recovery.
The next question concerns the choice of tactics for a safe approach to the midbrain area.
Dorsal lesions are localized in the zones of two thin horizontal lines immediately above and below the quadrigeminal plate. For their surgical treatment, supratentorial suboccipital, occipital transtentorial, supracerebellar infratentorial, posterior subtemporal and tonsillouveal transaqueductal approaches are used [14].
In the presented case, the infratentorial approach to the posterior fossa was used to remove the midbrain CM – this method is most often used by leading neurosurgeons around the world such as M. Lawton and R. Spetzler [3–5]. The two principal craniotomies were used to access the posterior fossa: retrosigmoid (lateral suboccipital) craniotomy and medial suboccipital craniotomy. The retrosigmoid supracrebellar approach was used to reach the lateral midbrain. The medial suboccipital supracrebellar approach was used to reach the dorsal part of the midbrain and the quadrigeminal plate [15].
The surgical tactics used in the subacute period of hemorrhage from the cavernoma allowed for radical removal of the midbrain CM, ensuring complete neurological recovery of the patient. The patient was able to carry on with his work as usual and there were no signs of a reoccurring hemorrhage (the observation time was 6.5 months).
Knowledge of the brainstem corridors is necessary for planning microsurgical interventions on brainstem formations so as to minimize the risk of damage to nearby structures.
CONCLUSION
The subacute phase of midbrain CM bleeding may be the best time for surgical resection of the cavernoma. The contralateral supracerebellar infratentorial approach is one of the available options for resection of dorsal midbrain CM. It can be considered if the formation is located behind the cerebral peduncle, facing the intrapeduncular fossa and interpeduncular cistern and extends to the dorsal side.
AUTHORS CONTRIBUTIONS
Narzullo O. Rahimov and Khurshed J. Rakhmonov performed surgical treatment and developed the concept of scientific work. Dzhumaboy R. Sanginov, Mahmarajab A. Khasanov developed the methodology for selecting and describing CT and MRI images. Narzullo O. Rahimov collected the material and analyzed the literature data. All authors approved the final version of the publication.
ВКЛАД АВТОРОВ
Н.О. Рахимов и Х.Д. Рахмонов провели хирургическое лечение и разработали концепцию научной работы. Д.Р. Сангинов, М.А. Хасанов отвечали за подбор и описание снимков КТ и МРТ. Н.О. Рахимов осуществил сбор материала и анализ литературных данных. Все авторы одобрили окончательную версию публикации.
Compliance with ethical standards. Consent statement. The patient consented to the publication of the article “Microsurgical removal of a cavernous malformation on the midbrain dorsal surface using the supracerebellar infratentorial approach: а clinical case” in the “Sechenov Medical Journal”.
Conflict of interests. The authors declare that there is no conflict of interest.
Financing. The study was not sponsored (own resources).
Соблюдение этических норм. Заявление о согласии. Пациент дал согласие на публикацию представленной статьи «Микрохирургическое удаление кавернозной мальформации дорсальной поверхности среднего мозга путем супрацеребеллярного инфратенториального доступа: клинический случай» в журнале «Сеченовский вестник».
Конфликт интересов. Авторы заявляют об отсутствии конфликта интересов.
Финансирование. Исследование не имело спонсорской поддержки (собственные ресурсы).
1. Index of Clinical Guidelines by the Russian Ministry of Health / Clinical Guidelines / Mononeuropathies (Approved by the Ministry of Health of the Russian Federation) https://cr.minzdrav.gov.ru/preview-cr/166_2 (access date: 13.05.2024).
References
1. S1. Snellings D.A., Hong C.C., Ren A.A., et al. Cerebral Cavernous Malformation: From Mechanism to Therapy. Circ Res. 2021 Jun 25; 129(1): 195–215. https://doi.org/10.1161/CIRCRESAHA.121.318174. Epub 2021 Jun 24. Erratum in: Circ Res. 2021 Aug 6; 129(4): e101. https://doi.org/10.1161/RES.0000000000000496. PMID: 34166073
2. Tu T., Peng Z., Ren J., Zhang H. Cerebral Cavernous Malformation: Immune and Inflammatory Perspectives. Front Immunol. 2022 Jun 30; 13: 922281. https://doi.org/10.3389/fimmu.2022.922281. PMID: 35844490
3. Garcia R.M., Ivan M.E., Lawton M.T. Brainstem cavernous malformations: surgical results in 104 patients and a proposed grading system to predict neurological outcomes. Neurosurgery. 2015 Mar; 76(3): 265-277; discussion 277–278. https://doi.org/10.1227/NEU.0000000000000602. PMID: 25599905
4. Deshmukh V.R., Rangel-Castilla L., Spetzler R.F. Lateral inferior cerebellar peduncle approach to dorsolateral medullary cavernous malformation. J Neurosurg. 2014 Sep; 121(3): 723–729. https://doi.org/10.3171/2014.5.JNS132276. Epub 2014 Jun 27. PMID: 24972129
5. de Oliveira J.G., Lekovic G.P., Safavi-Abbasi S., et al. Supracerebellar infratentorial approach to cavernous malformations of the brainstem: surgical variants and clinical experience with 45 patients. Neurosurgery. 2010 Feb; 66(2): 389–399. https://doi.org/10.1227/01.NEU.0000363702.67016.5D. PMID: 20042987
6. Hong T., Xiao X., Ren J., et al. Somatic MAP3K3 and PIK3CA mutations in sporadic cerebral and spinal cord cavernous malformations. Brain. 2021 Oct 22; 144(9): 2648–2658. https://doi.org/10.1093/brain/awab117. PMID: 33729480
7. Rustenhoven J., Tanumihardja C., Kipnis J. Cerebrovascular Anomalies: Perspectives From Immunology and Cerebrospinal Fluid Flow. Circ Res. 2021 Jun 25; 129(1): 174–194. https://doi.org/10.1161/CIRCRESAHA.121.318173. Epub 2021 Jun 24. PMID: 34166075
8. Jong-A-Liem G.S., Martins Sarti T.H., Fernandes Lima J.V., et al. Midbrain Cavernous Malformation: Microsurgical Nuances and an Anatomoclinical Review 2-Dimensional Video. World Neurosurg. 2024 Nov; 191: 23–24. https://doi.org/10.1016/j.wneu.2024.07.213. Epub 2024 Aug 8. PMID: 39122114
9. Kurihara N., Suzuki H., Kato Y., et al. Hemorrhage owing to cerebral cavernous malformation: imaging, clinical, and histopathological considerations. Jpn J Radiol. 2020 Jul; 38(7): 613–621. https://doi.org/10.1007/s11604-020-00949-x. Epub 2020 Mar 27. PMID: 32221793
10. Joseph N.K., Kumar S., Brown R.D. Jr., et al. Influence of Pregnancy on Hemorrhage Risk in Women With Cerebral and Spinal Cavernous Malformations. Stroke. 2021 Jan; 52(2): 434– 441. https://doi.org/10.1161/STROKEAHA.120.031761. Epub 2021 Jan 25. PMID: 33493052
11. Spetzler R.F., Martin N.A. A proposed grading system for arteriovenous malformations. J Neurosurg. 1986 Oct; 65(4): 476–483. https://doi.org/10.3171/jns.1986.65.4.0476. PMID: 3760956
12. Lawton M.T., Kim H., McCulloch C.E. et al. A supplementary grading scale for selecting patients with brain arteriovenous malformations for surgery. Neurosurgery. 2010 Apr; 66(4): 702–713; discussion 713. https://doi.org/10.1227/01.NEU.0000367555.16733. E1. PMID: 20190666
13. Negoto T., Terachi S., Baba Y., et al. Symptomatic Brainstem Cavernoma of Elderly Patients: Timing and Strategy of Surgical Treatment. Two Case Reports and Review of the Literature. World Neurosurg. 2018 Mar; 111: 227–234. https://doi.org/10.1016/j.wneu.2017.12.111. Epub 2017 Dec 27. PMID: 29288846
14. Phi J.H., Kim S.K. Clinical Features and Treatment of Pediatric Cerebral Cavernous Malformations. J Korean Neurosurg Soc. 2024 May; 67(3): 299–307. https://doi.org/10.3340/jkns.2024.0047. Epub 2024 Mar 28. Erratum in: J Korean Neurosurg Soc. 2024 Jul; 67(4): 486. https://doi.org/10.3340/jkns.2024.0047.e1. PMID: 38547881
15. Ma L., Zhang S., Li Z.,, et al. Morbidity After Symptomatic Hemorrhage of Cerebral Cavernous Malformation: A Nomogram Approach to Risk Assessment. Stroke. 2020 Oct; 51(10): 2997– 3006. https://doi.org/10.1161/STROKEAHA.120.029942. Epub 2020 Sep 21. PMID: 32951540
About the Authors
N. O. RahimovTajikistan
Narzullo O. Rahimov, Cand. of Sci. (Medicine), Associate Professor, Department of Neurosurgery and Combined Trauma; neurosurgeon of the Department of Neurosurgery
29–31, Sino Ave., Sino str., Dushanbe, 734003,
59, I. Somoni Ave., Dushanbe, 734026
K. J. Rakhmonov
Tajikistan
Khurshed J. Rakhmonov, Dr. of Sci. (Medicine), Professor, Department of Neurosurgery and Combined Trauma; Director
29–31, Sino Ave., Sino str., Dushanbe, 734003,
59, I. Somoni Ave., Dushanbe, 734026
D. R. Sanginov
Tajikistan
Dzhumaboy R. Sanginov, Dr. of Sci. (Medicine), Professor, Department of Oncology
29–31, Sino Ave., Sino str., Dushanbe, 734003
M. A. Khasanov
Tajikistan
Mukhamadrajab A. Khasanov, resident, Department of Neurosurgery and Combined Trauma
29–31, Sino Ave., Sino str., Dushanbe, 734003
Supplementary files

|
1. 1210-CARE checklist | |
| Subject | ||
| Type | Исследовательские инструменты | |
Download
(107KB)
|
Indexing metadata ▾ | |
Review
Sechenov Medical Journal. Editor's checklist for this article you can find here.
Журнал «Сеченовский вестник» |
| Sechenov Medical Journal |
Рецензии на рукопись |
| Peer-review reports |
Название / Title | Микрохирургическое удаление кавернозной мальформации дорсальной поверхности среднего мозга путем супрацеребеллярного инфратенториального доступа: клинический случай / Microsurgical removal of a cavernous malformation on the midbrain dorsal surface using the supracerebellar infratentorial approach: а clinical case |
Раздел / Section
| НЕЙРОХИРУРГИЯ/ NEUROSURGERY
|
Тип / Article | Клинический случай / Сlinical case |
Номер / Number | 1210
|
Страна/территория / Country/Territory of origin | Россия / Russia |
Язык / Language | Английский /Русский/ English/Russian
|
Источник / Manuscript source | Инициативная рукопись / Unsolicited manuscript |
Дата поступления / Received | 12.05.2025 |
Тип рецензирования / Type ofpeer-review | Двойное слепое / Double blind |
Язык рецензирования / Peer-review language | Русский / Russian |
РЕЦЕНЗЕНТ А / REVIEWER A
Инициалы / Initials | 1210_А
|
Научная степень / Scientific degree | Кадидат медицинских наук / Cand. of Sci. (Medicine)
|
Страна/территория / Country/Territory | Россия / Russia
|
Дата рецензирования / Date of peer-review | 09.06.2025 |
Число раундов рецензирования / Number of peer-review rounds | 1 |
Финальное решение / Final decision | принять к публикации / accept
|
ПЕРВЫЙ РАУНД РЕЦЕНЗИРОВАНИЯ / FIRST ROUND OF PEER-REVIEW
Представленный клинический случай микрохирургического удаления кавернозной мальформации дорзальной поверхности среднего мозга из супрацеребеллярного - инфратенториального доступа отражает высокий профессионализм авторов при выборе тактики лечения данной патологии. Авторам удалось успешно прооперировать 38-летнего пациента с вышеуказанной патологией добиться регресса неврологической симптоматики.
В представленной работе полностью дана характеристика самой патологии, использованы современные методы диагностики и нейровизуализации, что наглядно показывают приведённые иллюстрации.
Следует подчеркнуть, что успех операции зависит от тщательной предоперационной подготовки всей команды. Авторы сравнивали всевозможные доступы к данной зоне и выбрали самый оптимальный доступ
Имеются незначительные орфографические ошибки и неточности при оформлении рукописи, что требует корректировки.
ЗАКЛЮЧЕНИЕ: принять к публикации
РЕЦЕНЗЕНТ B / REVIEWER B
Инициалы / Initials | 1210_В
|
Научная степень / Scientific degree | Кандидат медицинских наук / Cand. of Sci. (Medicine) |
Страна/территория / Country/Territory | Россия / Russia
|
Дата рецензирования / Date of peer-review | 12.06.2025 |
Число раундов рецензирования / Number of peer-review rounds | 1 |
Финальное решение / Final decision | Отклонить / Decline
|
ПЕРВЫЙ РАУНД РЕЦЕНЗИРОВАНИЯ / FIRST ROUND OF PEER-REVIEW
Представленная работа, посвящённая клиническому случаю хирургического лечения кавернозной мальформации области таламуса и среднего мозга, представляет определённый практический интерес благодаря детальному описанию планирования вмешательства, хода операции и благоприятного исхода для пациента.
Вместе с этим рукопись нуждается в доработке по ряду аспектов. По данным МРТ определяется крупная кавернозная мальформация левого таламуса с вовлечением дорсальной части среднего мозга. Текст содержит значительное количество языковых и стилистических неточностей, что затрудняет восприятие описания хирургического вмешательства. Рекомендуется привести анатомическую терминологию в соответствие с международными стандартами (PNA) и уточнить формулировки. Например, фразу «Соединительные вены к тенториуму разделяются, чтобы открыть коридор к свободному краю тенториума. Арахноидальная оболочка заднего резцового пространства рассекали, чтобы дренировать четверохолмную цистерну и обнажить дорзальную часть среднего мозга» целесообразно переформулировать следующим образом: «Для доступа к свободному краю намёта мозжечка были пересечены мостиковые вены между мозжечком и наметом. Далее выполнена диссекция паутинной оболочки заднего отдела четверохолмной цистерны для визуализации дорсальной поверхности среднего мозга».
Следует отметить, что использованный хирургический доступ является достаточно хорошо описанным и широко применяемым в нейрохирургической практике, и в представленном случае авторам было бы важно более чётко обозначить, в чём именно состоит оригинальность их технического решения, если она предполагается. В описании клинической картины целесообразно уточнить сторону косоглазия и отразить элементы альтернирующего синдрома, что сделает неврологический статус более понятным для читателя. Комментарии к иллюстрациям нуждаются в расширении и уточнении с расшифровкой всех обозначений. Отдельного уточнения требует также применённая классификация каверном – рекомендуется использовать классификации, принятые для кавернозных мальформаций ствола головного мозга.
В целом рукопись имеет потенциал, однако требует существенной доработки с учётом указанных замечаний. После внесения соответствующих исправлений и возможной корректировки названия рекомендуется повторная подача материала на рассмотрение.
ЗАКЛЮЧЕНИЕ: отклонить статью.
РЕКОМЕНДАЦИИ НАУЧНЫХ РЕДАКТОРОВ ЖУРНАЛА / RECOMMENDATIONS
OF THE SCIENTIFIC EDITORS OF THE JOURNAL
Ключевые слова
- Необходимо добавить 5–8 ключевых слов, которые обеспечат корректное индексирование статьи в базах данных и повысит её видимость в научных поисковых системах. При этом ключевые слова не должны напрямую повторять формулировки, используемые в названии рукописи.
Ключевые положения
- Следует добавить три ключевых положения, отражающих наиболее важные выводы и практическую значимость статьи. Это позволит читателю быстро понять, какие новые знания и клинические выводы можно получить из представленной работы.
Введение
- Требуется чётко сформулировать новизну исследования (например, как первый клинический опыт в Таджикистане) и обосновать значимость публикации именно данного клинического случая, что усилит научную и практическую ценность рукописи.
- Цель описания клинического случая должна быть сформулирована ясно и размещена в последнем абзаце введения, что обеспечит логическую завершённость и структурированность раздела.
Основной текст
- Необходимо указать уровень сознания по шкале комы Глазго, а также уточнить сторону косоглазия, наличие мидриаза и паралича аккомодации, поскольку эти данные важны для объективной оценки неврологического статуса пациента.
- Описание хода операции рекомендуется структурировать по этапам, что повысит ясность изложения и облегчит восприятие материала читателем.
Язык
- Текст на русском языке требует значительного литературного и стилистического редактирования, включая согласование падежных форм и лексико-грамматическую корректность предложений, что необходимо для повышения читаемости и академического уровня рукописи.
- Все анатомические термины должны быть приведены в соответствии с Парижской анатомической номенклатурой (PNA), что обеспечит международную стандартизацию терминологии.
Рисунки
- Изображения, представленные на рисунке 2, необходимо отсканировать в высоком качестве с одинаковыми параметрами яркости и контрастности. Каждое изображение должно быть предоставлено отдельным файлом, что требуется для качественной верстки и публикации.
- В подписях к рисункам следует подробно описать все выявленные изменения, а на самих изображениях обозначить их стрелками, что повысит информативность и научную ценность иллюстраций.
- Рисунки необходимо предоставить в отдельных файлах с соблюдением требований к оформлению изображений, размещённых на сайте журнала, что обеспечит их соответствие техническим стандартам издания.
Список литературы
- Для всех классификаций, используемых в тексте (IV/V степени по классификации Medical Research Council, Spetzler–Martin IV, хирургическая стратегия по M. Lawton–Young III, Grade 7), необходимо привести ссылки в виде сносок, и не включать их в основной список литературы, поскольку они используются в качестве описательных шкал.
- Для всех источников следует добавить идентификаторы DOI и PMID, что необходимо для корректной индексации и проверки источников в международных базах данных.
- Для источника № 8 необходимо указать ISBN, что обеспечит его точную идентификацию.
- Список литературы должен быть оформлен в соответствии с требованиями журнала (раздел 5.7: что является обязательным условием для публикации рукописи.
JATS XML