Scroll to:
Intradural sequestration of lumbar disc herniation with cranial migration: a case report
https://doi.org/10.47093/2218-7332.2024.15.4.51-58
Abstract
Intradural herniation of the intervertebral disc (IHID) is extremely rare. There are only a few reports of cranial migration of an intradural fragment of a sequestered disc herniation.
Clinical case. A 51-year-old patient who had previously undergone two operations at L5–S1 and L4–L5 levels was admitted to the hospital with complaints of low back pain with radiation to both legs, numbness in the perineum and inner surface of the thighs, urinary retention, constipation. Magnetic resonance imaging revealed a 30 mm mass located at the level of the L3 vertebral body, within the dural sac and filling its entire transverse diameter. The cauda equina nerve roots were compressed. Surgery was performed: the herniated sequestrum (30×10×10 mm) was separated from the nerve roots fixed to it and removed. After surgery, sensation in the buttocks and inner thighs returned, and urinary urge appeared. Rehabilitation is ongoing.
Discussion. In most cases, IHID is diagnosed intraoperatively. In the presented case, the genesis of the formation remained unclear before surgery, so a laminectomy approach was chosen, which allowed for extensive revision of the intradural space, thorough radiculolysis, and identification of the cranial migration of the sequestrated disc herniation. The only effective treatment for IHID is surgery.
Keywords
Abbreviations:
- IHID – intradural herniation of the intervertebral disc
- Dura Mater – dural membrane
- MRI – magnetic resonance imaging
Intradural herniation of the intervertebral disc (IHID) is a rare pathology, with only a few hundred cases reported [1]. Most of these are described as isolated case reports. According to domestic studies, an analysis of 5435 patients with intervertebral disc herniation revealed that intradural migration at the L3–L4 segment accounted for 0.02% of cases [2].
The pathology is more common in men, with an average patient age of 50 to 60 years [1]. Among cases of intradural disc herniation, 92% occur in the lumbar spine, 5% in the thoracic region, and 3% in the cervical region [3]. Intradural involvement is most frequently observed at the L4–L5 level (55% of cases), followed by L3–L4 (16%) and L5–S1 (10%), with upper lumbar segments rarely affected [4].
This report presents a rare case of cranial migration of an intradural sequestered lumbar disc herniation.
CASE REPORT
A 45-year-old male patient underwent microdiscectomy for an L5–S1 herniated disc with S1 radiculopathy on the right side in 2008. Postoperatively, he experienced intermittent lower back pain, radiating along the lateral surface of the right thigh and shin, which increased in intensity and frequency in 2023.
MRI performed in February 2024 revealed a right-sided dorsolateral L4–L5 herniated disc with signs of sequestration, along with an L5–S1 disc extrusion (Figure 1). Surgical treatment was planned.
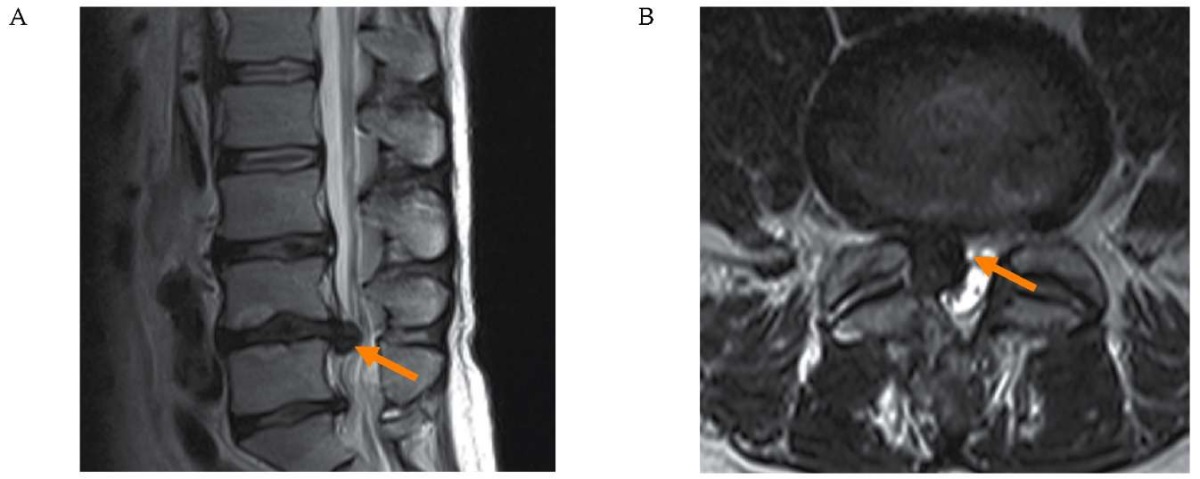
FIG. 1. Magnetic resonance imaging of the lumbar spine dated February 13, 2024, of a 51-year-old patient with a right-sided dorsolateral L4–L5 disc herniation.
A. Sagittal T2-weighted image.
B. Axial T2-weighted image through the disc herniation.
Right-sided dorsolateral L4–L5 disc herniation (orange arrow).
РИС. 1. Магнитно-резонансная томография пояснично-крестцового отдела позвоночника от 13.02.2024 пациента 51 года с правосторонней дорзо-латеральной грыжей диска L4–L5.
А. Т2 сагиттальный срез.
B. Т2 аксиальный срез, проходящий через грыжу.
Правосторонняя дорзо-латеральная грыжа диска L4–L5 (оранжевая стрелка).
In late February 2024, the patient experienced sudden, severe lower back pain radiating along the posterior surface of both legs. He subsequently developed perineal, gluteal, and inner thigh numbness, urinary retention, and constipation. Following these symptoms, he sought consultation at a medical center where a percutaneous endoscopic transforaminal discectomy was performed at the L4–L5 level on the right side. Postoperatively, pain along the lateral surface of the right thigh and shin resolved, but perineal numbness, bilateral posterior leg pain, and urinary retention persisted. In April 2024, he was hospitalized in the neurosurgery department at the Kozhevnikov Neurology Clinic.
Neurological examination revealed preserved motor function, reduced knee reflexes (D > S), severely diminished Achilles reflexes, and hypoesthesia in the perineum, inner thighs, buttocks, and right L5 dermatome. Tension signs were negative. Bladder dysfunction persisted, requiring abdominal muscle strain for urination, with minimal post-void residual urine (< 50 mL). Bowel movements occurred only with enemas.
Repeat MRI revealed a 30-mm intradural space-occupying lesion at the L3 level, completely filling the dural sac and compressing the cauda equina nerve roots (Figure 2). The lesion did not enhance with contrast.
A multidisciplinary consultation (neurologist, neurosurgeon, neuroradiologist) diagnosed a probable organized hematoma (ICD 10 code – I60.9). Surgery was indicated for spinal canal revision at L3.
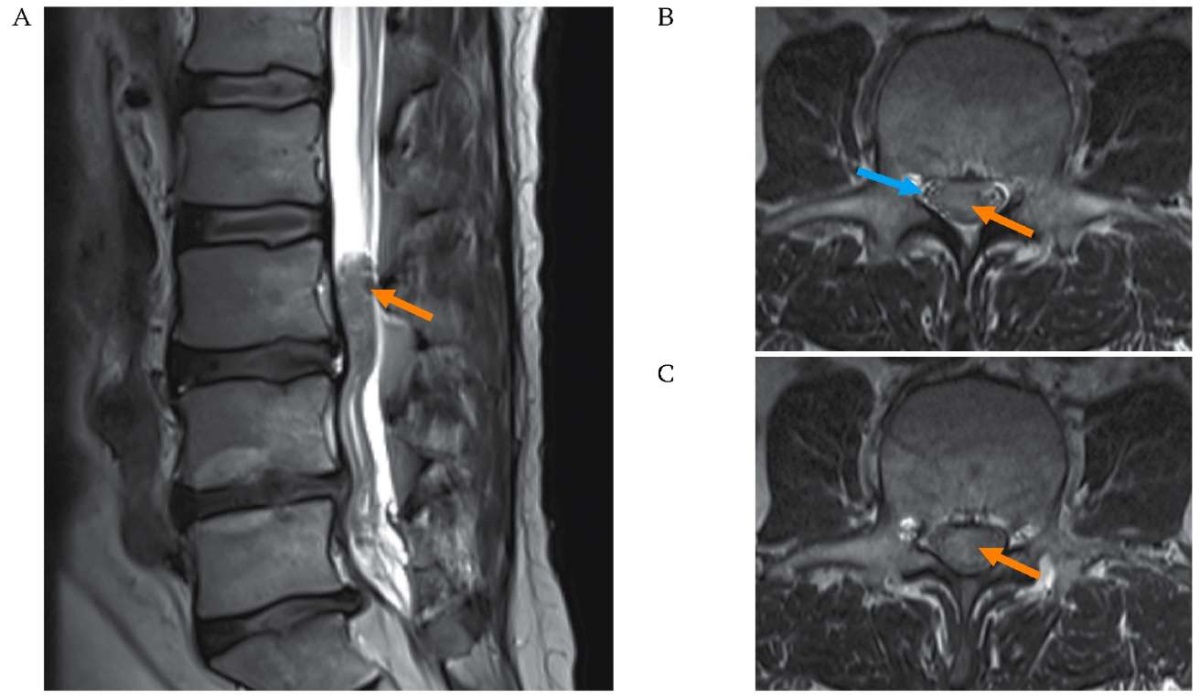
FIG. 2. Magnetic resonance imaging dated April 24, 2024, of a 51-year-old patient with an intradural space-occupying lesion in the spinal canal.
A. Sagittal T2-weighted image.
B. Axial T2-weighted image at the level of the middle thirds of the L3 vertebral body.
C. Axial T2-weighted images at the level of the lower thirds of the L3 vertebral body.
A 30 mm long intradural mass in the spinal canal at the level of L3 fills the entire cross-section of the dural sac (orange arrows). The cauda equina nerve roots are severely compressed and displaced to the periphery of the mass (blue arrow).
РИС. 2. Магнитно-резонансная томография от 24.04.2024 пациента 51 года с интрадуральным объемным образованием в позвоночном канале.
А. Т2 сагиттальный срез.
В. Т2 аксиальный срез на уровне средней трети тела L3.
С. Т2 аксиальный срез на уровне нижней трети тела L3.
Интрадуральное объемное образование в позвоночном канале протяженностью 30 мм на уровне L3 заполняет весь позвоночный канал (оранжевые стрелки). Корешки конского хвоста грубо компримированы, распределяются по периферии образования (голубая стрелка).
Surgery Procedure
On May 7, 2024, an L3 laminectomy and lower arcotomy of the L2 vertebra were performed. The dura mater (DM) was tense and non-pulsatile. Intraoperative ultrasound scanning of the affected cauda equina segment through the dura mater was performed (Figure 3A). A ventrally located intradural mass was identified, which did not extend beyond the laminectomy window. The dura mater was incised using a linear midline approach: the arachnoid membrane appeared thickened and cloudy, with adherent nerve roots (arachnopathy). Radiculolysis was performed, after which the herniated sequestrum was separated from the nerve roots and removed (Figures 3B, 3C). The sequestrum measured 30 × 10 × 10 mm. No defects in the anterior surface of the dural sac were found at the surgical site. The surgical wound was sutured layer by layer.
After surgery, there was a regression of pain in the lower back and legs and a reduction in the severity of hypoesthesia. Follow-up MRI on May 8, 2024, confirmed complete sequestrum removal (Figure 3D). The patient was discharged for outpatient care five days after surgery.
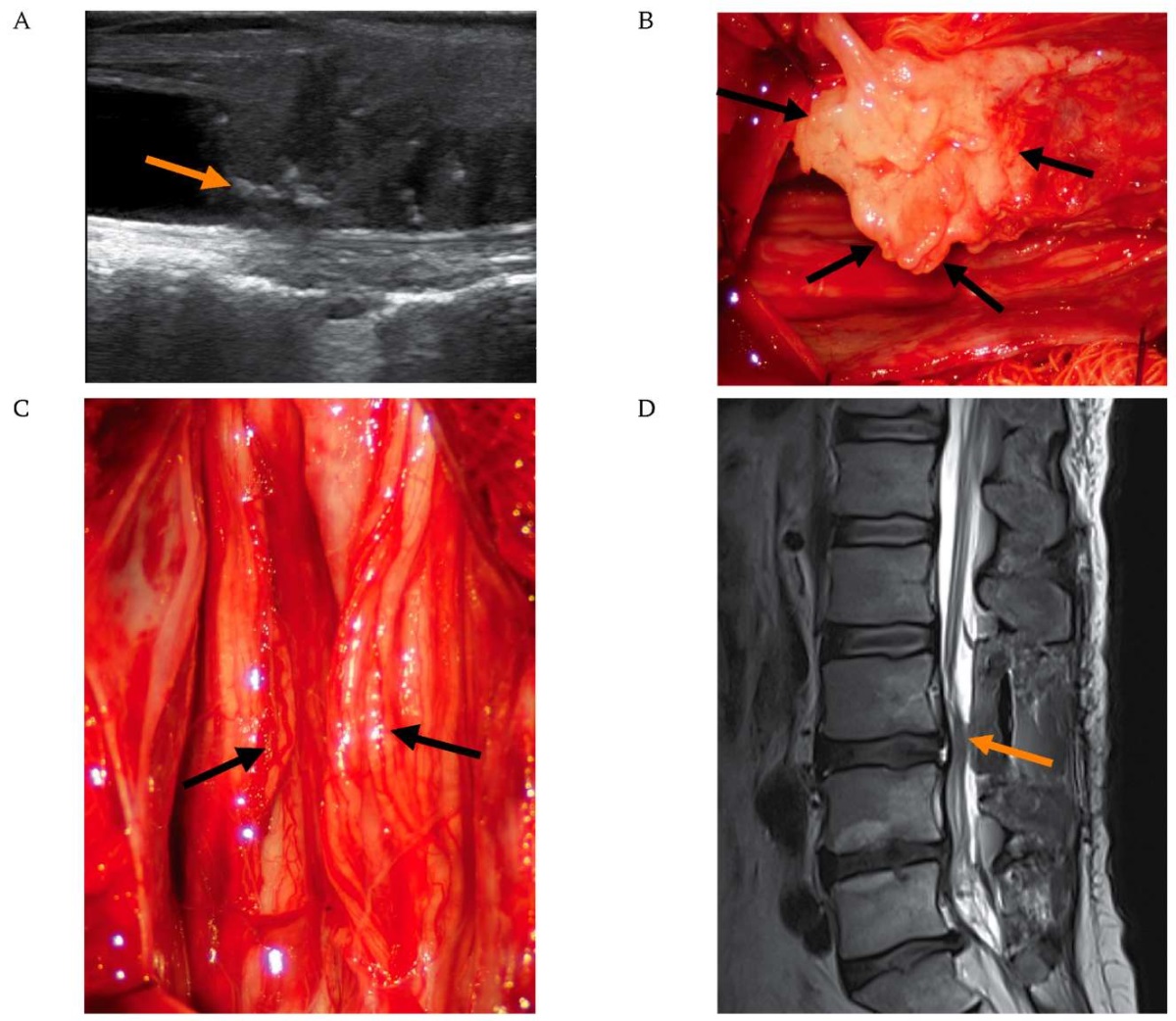
FIG. 3. Surgery to remove the intradural disc sequestrum in a 51-year-old patient, May 7, 2024.
A. Intraoperative ultrasound of the cauda equina nerve roots. Ultrasound was performed in the sagittal plane through the durotomy of the dural sac after L3 laminectomy. The hyperechoic area, marked by the orange arrow – represents the disc sequestrum.
B. Intraoperative micrograph. The sequestrum is dissected from adhesions and separated from the spinal nerve roots (black arrows).
C. Intraoperative micrograph. View of the spinal nerve roots after sequestrum removal (black arrows).
D. Postoperative lumbar spine magnetic resonance imaging performed the day after surgery: sagittal T2-weighted image. The sequestrum is completely removed (orange arrow).
РИС. 3. Операция удаления интрадурального грыжевого секвестра у пациента 51 года 07.05.2024.
A. Интраоперационное УЗ-сканирование корешков конского хвоста в сагиттальной плоскости через твердую мозговую оболочку дурального мешка после ламинэктомии L3 позвонка. Гиперэхогенная зона, обозначенная оранжевой стрелкой – грыжевой секвестр.
B. Интраоперационная микрофотография. Секвестр выделен из спаек и отделен от корешков спинного мозга (черные стрелки).
C. Интраоперационная микрофотография. Вид корешков спинного мозга после удаления секвестра (черные стрелки).
D. Магнитно-резонансная томография поясничного отдела позвоночника, выполненная на следующий день после операции: Т2 сагиттальный срез. Секвестр полностью удален (оранжевая стрелка).
At the time of writing (1.5 months post-surgery), the patient reports improved sensitivity in the buttocks and inner thighs and the return of urinary urgency. However, spontaneous urination remains possible only with abdominal muscle straining, and bowel movements still require enemas. Rehabilitation is ongoing.
DISCUSSION
Most authors agree that adhesions between the ventral part of the dural sac and the posterior longitudinal ligament are the primary factor contributing to the development of an intradural herniation [5]. Adhesion formation can result from degenerative disc disease, trauma, previous surgery, or inflammation [6–8]. This process leads to the fixation of the dural sac to the posterior longitudinal ligament and the outer portions of the annulus fibrosus. Movements in the lumbar spine cause an erosive process, thinning the fixed section of the dura mater [4][5].
A sudden excessive load can result in perforation of the dura mater, allowing the herniated disc to penetrate the intradural space [8]. Adhesions prevent the lateral migration of disc fragments in the case of sequestration [9].
Z. Tempel et al. described a patient with an intradural disc herniation at the L2–L3 level without epidural adhesions. They suggested that acute marginal osteophytes on the posterior vertebral bodies led to the thinning and rupture of the dura mater during disc sequestration [10]. D. Luo et al., during surgery, found an extra-intradural location of the herniation, with a significant portion of the sequestered disc tissue inside the dural sac and the rest in the epidural space [8]. Transdural penetration of herniated fragments has also been reported [7][11][12]. A possible mechanism of transdural rupture is the presence of a chronic, extensive intradural herniation, which leads to the thinning and subsequent rupture of the dorsal dura mater [7][11]. Thus, a stepwise migration of the herniation can be observed, from the ventral epidural space to the intradural space and then dorsally [8][13].
Migration of herniated fragments within the dural sac to other spinal segments is rarely described [10][14–18]. S. D. Daffner et al. were the first to report intraoperative migration of such a herniation, suggesting that it may have been caused by the patient’s position on the Wilson frame [17]. No reports of cranial migration of sequestra were found in domestic literature. In our case, it was impossible to determine the exact cause of cranial migration. It is likely that an awkward movement triggered the migration, leading to signs of cauda equina compression.
It has been noted that 30–60% of patients with intradural disc herniation (IDDH) present with cauda equina syndrome, a rate several times higher than that observed in epidural disc herniations [2][24]. Otherwise, the symptoms remain nonspecific [10].
IDDH is diagnosed intraoperatively in most cases [19], with only 7% of cases being identified preoperatively [20]. No specific MRI findings have been described to indicate intradural sequestration. However, in chronic IDDH cases, MRI with intravenous contrast may reveal a hyperintense granulation tissue rim, while the sequestrum itself does not accumulate contrast [21][22], which was observed in our patient.
Surgical intervention is the only effective treatment for IDDH [8]. In cases of cauda equina syndrome, urgent surgical decompression is required [10][23].
It is not possible to standardize the optimal surgical approach for IDDH removal, as in most cases, intradural penetration of the herniation is only identified during surgery. K. Kobayashi et al. suggest that in such cases, the surgical approach should be expanded to ensure reliable dura mater sealing [25].
In our clinical case, the etiology of the herniation remained unclear before surgery, so a laminectomy was chosen as the surgical approach. This allowed for a thorough revision of the intradural space, meticulous radiculolysis, and the identification of cranial migration of the sequestered disc herniation. The operation was performed approximately nine weeks after the suspected penetration of disc material into the intradural space. The prolonged presence of the sequestrum in the terminal cistern led to severe arachnopathy, complicating herniation removal and limiting the degree of clinical improvement postoperatively.
Dural defects resulting from intradural sequestration can be sutured without additional grafting, depending on their size and location, or closed using autologous tissue or allografts with additional sealing using biological glue [8][24]. In the presented case, sequestration penetrated the intradural space at the L4–L5 level and migrated into the dural sac to the L3 vertebral body level, where no dural defect was detected.
CONCLUSION
Cranial migration of an intradural sequestered disc herniation is an extremely rare pathology without specific clinical signs. MRI findings of a migrated sequestrum within the dural sac present as an intradural mass of uncertain etiology. The diagnosis is often made intraoperatively. Delayed sequestrum removal leads to severe arachnopathy, complicating surgical intervention.
AUTHORS CONTRIBUTIONS
Grigoriy Yu. Evzikov developed the main concept of the article, wrote the text, approved the final version, and agreed to take responsibility for all aspects of the case report. Mikhail G. Bashlachev and Maksim I. Gaydash participated in developing the concept of the article and drafting the text. Grigoriy Yu. Evzikov, Mikhail G. Bashlachev took an active part in the treatment of the patient. All authors approved the final version of the article.
ВКЛАД АВТОРОВ
Г.Ю. Евзиков внес основной вклад в разработку концепции статьи, подготовил текст и согласен принять на себя ответственность за все аспекты клинического наблюдения. М.Г. Башлачев и М.И. Гайдаш участвовали в разработке концепции статьи и подготовке текста. Г.Ю. Евзиков, М.Г. Башлачев принимали активное участие в лечении пациента. Все авторы одобрили окончательную версию статьи.
Ethics statements. Consent statement. The patient consented to the publication of the article “Intradural sequestration of lumbar disc herniation with cranial migration: a case report” in the “Sechenov Medical Journal”.
Conflict of interests. The authors declare that there is no conf ict of interests.
Financial support. The study was not sponsored (own resources).
Соответствие принципам этики. Заявление о согласии. Пациент дал согласие на публикацию представленной статьи «Интрадуральный секвестр межпозвонковой грыжи поясничного отдела позвоночника с краниальной миграцией: клиническое наблюдение» в журнале «Сеченовский вестник».
Конфликт интересов. Авторы заявляют об отсутствии конфликта интересов.
Финансирование. Исследование не имело спонсорской поддержки (собственные ресурсы).
References
1. Loya V.K., Krishna Narayan T.V., Singh Dhillon C., Shashikant Pophale C. Intradural lumbar disc herniation with cauda equina syndrome: Case report and recent advances. Brain Spine. 2023 Dec 14; 4: 102724. https://doi.org/10.1016/j.bas.2023.102724. PMID: 38510606
2. Байков Е.С., Крутько А.В. Грыжи межпозвонковых дисков с интрадуральной миграцией их фрагментов. Хирургия позвоночника. 2016; 13(4): 73–77. https://doi.org/10.14531/ss2016.4.73-77. EDN: XBKHFD / Baikov E.S., Krutko A.V. Intervertebral disc herniation with intradural migra tion of fragments. Russian Journal of Spine Surgery (Khirurgiya Pozvonochnika). 2016; 13(4): 73–77 (In Russian). https://doi.org/10.14531/ss2016.4.73-77. EDN: XBKHFD
3. Jin Y.Z., Zhao B., Zhao X.F., et al. Lumbar intradural disc herniation caused by injury: a case report and literature review. Orthop Surg. 2023 Jun; 15(6): 1694–1701. https://doi.org/10.1111/os.13723. PMID: 37073103
4. Wen H., Xiao L., Chen Y., et al. Intradural disc herniation at the L2/3 level: a case report and literature review. Annals of palliative medicine. 2022 Sep; 11(9): 3005–3013. https://doi.org/10.21037/apm-22-1017. PMID: 36217628
5. Floeth F., Herdmann J. Chronic dura erosion and intradural lumbar disc herniation: CT and MR imaging and intraoperative photographs of a transdural sequestrectomy. European spine J. 2012 Jun; 21 Suppl 4(Suppl 4): S453–457. https://doi.org/10.1007/s00586-011-2073-2. PMID: 22109565
6. Rathod T., Panchal S., Marathe N., et al. Intradural disc herniation in the lumbar spine: a case report. JNMA J. Nepal Med Assoc. 2020 May 30; 58(225): 345–348. https://doi.org/10.31729/jnma.4798. PMID: 32538932
7. Pedaballe A.R., Mallepally A.R., Tandon V., et al. An unusual case of transdural herniation of a lumbar intervertebral disc: diagnostic and surgical challenges. World Neurosurg. 2019 Aug; 128: 385–389. https://doi.org/10.1016/j.wneu.2019.05.103. PMID: 31121367
8. Luo D., Ji C., Xu H., et al. Intradural disc herniation at L4/5 level causing Cauda equina syndrome: A case report. Medicine (Baltimore). 2020 Feb; 99(7): e19025. https://doi.org/10.1097/MD.0000000000019025. PMID: 32049799
9. Theodorou D.J., Theodorou S.J., Kakitsubata Y., et al. P osterior and anterior epidural and intradural migration of the sequestered intervertebral disc: Three cases and review of the literature. J. Spinal Cord Med. 2022 Mar; 45(2): 305–310. https://doi.org/10.1080/10790268.2020.1730110. PMID: 32130089
10. Tempel Z., Zhu X., McDowell M.M., et al. Severe intradural lumbar disc herniation with cranially oriented free fragment migration. World Neurosurg. 2016 Aug; 92: 582.e1–582.e4. Epub 2016 Jun 16. https://doi.org/10.1016/j.wneu.2016.06.024. PMID: 27318310
11. Singh P.K., Shrivastava S., Dulani R., et al. Dorsal herniation of cauda equina due to sequestrated intradural disc. Asian Spine J. 2012 Jun; 6(2): 145–147. https://doi.org/10.4184/asj.2012.6.2.145. PMID: 22708020
12. Reina E.G., Calonge E.R., Heriot R.P. Transdural lumbar disc herniation. Spine (Phila Pa 1976). 1994 Mar 1; 19(5): 617–619. https:// doi.org/10.1097/00007632-199403000-00020. PMID: 8184359
13. Oztürk A., Avci E., Yazgan P., et al. Intradural herniation of intervertebral disc at the level of Lumbar 1-Lumbar 2. Turk Neurosurg. 2007 Apr; 17(2): 134–137. PMID: 17935031
14. Sarliève P., Delabrousse E., Clair C., et al. Intradural disc herniation with cranial migration of an excluded fragment. Clin Imaging. 2004 May-Jun; 28(3): 170–172. https://doi.org/10.1016/S0899-7071(03)00147-5. PMID: 15158220
15. Choi J.Y., Lee W.S., Sung K.H. Intradural lumbar disc herniation – is it predictable preoperatively? A report of two cases. Spine J. 2007 Jan-Feb; 7(1): 111–117. https://doi.org/10.1016/j.spinee.2006.02.025. PMID: 17197344
16. Kim H.S., Eun J.P., Park J.S. Intradural migration of a sequestrated lumbar disc fragment masquerading as a spinal intradural tumor. J. Korean Neurosurg Soc. 2012 Aug; 52(2): 156–158. https://doi.org/10.3340/jkns.2012.52.2.156. PMID: 23091677
17. Daffner S.D., Sedney C.L., Rosen C.L. Migratory intradural disk herniation and a strategy for intraoperative localization. Global Spine J. 2015 Feb; 5(1): 55–58. https://doi.org/10.1055/s-0034-1381728. PMID: 25648315
18. Park Y.S., Hyun S.J., Kim K.J., Jahng T.A. Multiple intradural disc herniations masquerading as intradural extramedullary tumors: a case report and review of the literature. Korean J. Spine. 2016 Mar; 13(1): 30–32. https://doi.org/10.14245/kjs.2016.13.1.30. PMID: 27123028
19. Cheng C.H., Che-Chao Chang M.P., Lin H.L., et al. Intradural lumbar disc herniation: A case report and literature review. Heliyon. 2022 Dec 14; 8(12): e12257. https://doi.org/10.1016/j.heliyon.2022.e12257. PMID: 36578377
20. Matsumoto T., Toyoda H., Terai H., et al. Utility of discography as a preoperative diagnostic tool for intradural lumbar disc herniation. Asian Spine J. 2016 Aug; 10(4): 771–775. https://doi.org/10.4184/asj.2016.10.4.771. PMID: 27559461
21. Wasserstrom R., Mamourian A.C., Black J.F., Lehman R.A. Intradural lumbar disk fragment with ring enhancement on MR. AJNR Am J. Neuroradiol. 1993 Mar-Apr; 14(2): 401–404. PMID: 8456719
22. Ihejirika R.C., Tong Y., Patel K., Protopsaltis T. Intradural lumbar disc herniation: illustrative case. J. Neurosurg Case Lessons. 2021 Nov 1; 2(18): CASE21336. https://doi.org/10.3171/CASE21336. PMID: 36061623
23. Arrigo R.T., Kalanithi P., Boakye M. Is cauda equina syndrome being treated within the recommended time frame? Neurosurgery. 2011 Jun; 68(6): 1520–1526; discussion 1526. https://doi.org/10.1227/NEU.0b013e31820cd426. Erratum in: Neurosurgery. 2012 May; 70(5): 1324–1325 . PMID: 21311382
24. Kobayashi K., Imagama S., Matsubara Y., et al. Intradural disc herniation: radiographic fi fi ndings and surgical results with a literature review. Clin Neurol Neurosurg. 2014 Oct; 125: 47–51. https://doi.org/10.1016/j.clineuro.2014.06.033. PMID: 25086430
25. Huliyappa H.A., Singh R.K., Singh S.K., et al. Transdural herniated lumbar disc disease with muscle patch for closure of durotomy – A Brief review of literature. Neurol Neurochir Pol. 2017 Mar-Apr; 51(2): 149–155. https://doi.org/10.1016/j.pjnns.2016.12.002. PMID: 28024891
About the Authors
Grigoriy Yu. EvzikovRussian Federation
Grigoriy Yu. Evzikov – Doctor of Sci. (Medicine), Professor, Department of Nervous Diseases and Neurosurgery,
8/2, Trubetskaya str., Moscow, 119048.
Mikhail G. Bashlachev
Russian Federation
Mikhail G. Bashlachev – Cand. of Sci. (Medicine), neurosurgeon, Neurosurgical Department with an Operating Unit, Kozhevnikov Clinic of Nervous Diseases, University Clinical Hospital No. 3,
8/2, Trubetskaya str., Moscow, 119048.
Maksim I. Gaydash
Russian Federation
Maksim I. Gaydash, Maksim I. Gaydash – neurologist, postgraduate student, Department of Nervous Diseases and Neurosurgery,
8/2, Trubetskaya str., Moscow, 119048.
Supplementary files

|
1. CARE Checklist | |
| Subject | ||
| Type | Research Instrument | |
Download
(114KB)
|
Indexing metadata ▾ | |







































