Scroll to:
Ultrasonography cervical volume as a predictor of successful induction of labor: a systematic review and meta-analysis
https://doi.org/10.47093/2218-7332.2025.1223
Abstract
Aim. To compare the cervical volume of patients who underwent successful and failed induction of labor (IOL) procedures.
Materials and methods. This systematic review and meta-analysis were conducted according to PRISMA guidelines. A comprehensive literature search was performed in PubMed, EMBASE, Scopus, and Google Scholar to identify cohort studies published between January 01, 2005 and December 31, 2024, that compared cervical volume in pregnant women who underwent IOL. A random-effects meta-analysis was performed.
Results. Seven studies involving 534 pregnant women were included. Four studies were considered low risk of bias and two studies were regarded as high risk of bias. Risk of bias assessment could not be performed in one study because the full-text of the article was not available. The pooled analysis of two studies involving 168 pregnant women demonstrated a positive association between the lower cervical volume and successful vaginal delivery within 24 hours (odds ratio 7.19; 95% confidence interval: 3.31 to 15.64; I² = 0%). The pooled analysis of five studies involving 422 pregnant women showed no statistically significant difference between successful and failed IOL, with a mean difference –1.32 cm3; 95% confidence interval: –8.37 to 5.72; I² = 89.8%). Subgroup analyses showed no statistically significant association between cervical volume and successful IOL when defined as vaginal delivery without time restriction or within 24 hours. However, a significantly lower cervical volume was observed in women who achieved the active phase of labor within 12 hours. The Egger’s regression test confirmed the absence of small‑study effects (coefficient = 0.50, standard error = 1.75, p = 0.78).
Conclusion. Cervical volume has significant potential as a parameter for predicting successful IOL, with a smaller cervical volume being associated with better outcomes, although subgroup findings remain inconsistent.
Abbreviations:
- CD – cesarean delivery
- CI – confidence interval
- IOL – induction of labor
- MD – mean difference
- OR – odds ratio
- VD – vaginal delivery
Induction of labor (IOL) is a common procedure in the field of obstetrics which is aimed at stimulating uterine contractions befo e the onset of labor to achieve vaginal delivery (VD) [1]. The World Health Organization reported in 2018 that the prevalence of IOL reaches 25% in developed countries1. However, IOL can lead to maternal and fetal morbidity and mortality [1]. It increases the risk of emergency cesarean delivery (CD) (odds ratio (OR) 1.89; 95% confidence interval (CI): 1.12 to 3.18) [2], chorioamnionitis (OR 2.6; 95% CI: 2.0 to 3.4) [3], postpartum hemorrhage (OR 1.57; 95% CI: 1.2 to 2.04), and uterine rupture or dehiscence at 1.1% (OR 1.62; 95% CI: 1.13 to 2.31) [4]. These risks emphasize the need for pre-induction assessment to predict successful IOL and minimize adverse outcomes.
The Bishop score is a bedside, pre-induction cervical assessment that sums dilation, effacement, station, position, and consistency to estimate the likelihood of successful IOL. However, because it relies on digital examination rather than objective imaging, it is inherently subjective with notable intra- and inter-observer variability [5][6], which has driven interest in ultrasound-based pre-induction assessments. Ultrasonographic cervical assessment is performed to assess pre-induction cervical ripening. Common sonographic parameters for predicting IOL success include cervical length, uterocervical angle, and cervical elastography which represents cervical stiffness.
Ultrasonographic cervical assessment shows promise, but prior studies report variable results, so its predictive value for IOL outcomes is not fully established [7–11]. Cervical volume, an alternative novel sonographic measure, may be a predictor of successful IOL. However, its efficacy in predicting successful IOL has not yet been thoroughly explored or reviewed.
Aim of the study: to compare the cervical volume of patients who underwent successful and failed IOL procedures.
MATERIALS AND METHODS
This systematic review and meta-analysis were conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) extension statement for reporting systematic reviews incorporating meta-analysis [12]. Preliminary data was presented at an international conference2.
Information sources
The databases search was performed covering all available studies, conference proceedings, dissertations, and theses published between January 01, 2005 and December 31, 2024. The studies were identified in PubMed, EMBASE, Scopus, and via manual searches using Google Scholar. The final search was conducted on March 28, 2025.
Eligibility criteria and search strategy
Search terms were developed based on the PECOS framework (population, exposure, comparator, outcomes, and study design)3. The full search strategy is presented in Supplement 1 (Supplementary materials on the journal’s website https://doi.org/10.47093/2218-7332.2025.1223-annex).
Inclusion criteria:
- Population: pregnant women who underwent IOL;
- Exposure: the measurement of cervical volume using ultrasonography via any route (transabdominal, transvaginal, or transperineal), with or without a specified cut-off value;
- Comparator: cervical volume threshold (for studies with a cut-off value);
- Outcome: at least one definition of successful IOL, characterized by: VD without a specified timeframe, VD within 24 hours, and achievement of the active phase of labor within 12 hours;
- Study design: cohort studies.
Non-inclusion criteria:
- Non-English languages that were untranslatable;
- The insufficient data for analysis despite three contact attempts with the authors spaced two weeks apart.
Selection process
Studies were manually and independently screened by two reviewers (P.K. and P.C.) based on the titles and abstracts, without the use of automation tools. The full articles were subsequently reviewed to confirm inclusion. Any disagreements were resolved through discussion with a third reviewer (M.S.).
Data collection process
Data was collected independently by two reviewers (P.K. and P.C.) using a standardized data extraction form. Extracted data comprised 6 sections: general study information, study characteristics, participant characteristics, ultrasonographic cervical volume assessment details, outcome summaries, and data for pooling. Study characteristics included the extraction date, author name, study location, ultrasound type and name of ultrasound machine, route of ultrasound, cervical volume measurement methods, participant demographics, method of IOL, indications of IOL, pregnancy complications, ultrasonographic cervical volume, and outcomes of IOL. The researchers classified ‘CD,’ ‘not achieving VD,’ and ‘no achievement of the active phase of labor’ as failed IOLs to avoid inconsistency.
Risk of bias assessment
Two reviewers (P.K. and P.C.) independently assessed the risk of bias in the studies using the modified Newcastle-Ottawa scale, a validated tool for assessing the quality of non-randomized studies4. This scale evaluates three domains of bias: selection of the representativeness of the study participants, comparability between groups, and ascertainment of outcomes and study factors. Each item contains a question with three possible answers: yes, no, or unclear. The scale assigns scores ranging from 0 to 9 stars. Individual studies were categorized according to these stars; those with 7 to 9 stars were classified as having a low risk of bias, those with 4 to 6 stars as having a moderate risk of bias, and those with 0 to 3 stars as having a high risk of bias. The third reviewer (M.S.) resolved any disagreements.
Data analysis
Data for pooling was divided into two types: cut-off data and frequency data. For studies with a cut-off, a comparator was implicitly defined (e.g., cervical volume above vs below the threshold), and the data were analyzed as binary outcomes using OR with 95% CI. For studies without a cut-off, cervical volume was considered as a continuous variable, and the data were pooled using mean difference (MD) with 95% CI. The cervical volume data was converted to mean and standard deviation when reported as a median, range, or interquartile range [13]. A random-effects meta-analysis was performed to account for potential heterogeneity across the trials. Leave-one-out sensitivity analyses were performed to assess the robustness of pooled estimates. Heterogeneity was assessed using Cochran’s Q test and Higgins’s I² statistic, where an I² more than 50% was considered indicative of substantial heterogeneity [14]. Meta-regression and subgroup analyses were pre-specified to explore potential sources of heterogeneity, including outcome definitions, measurement techniques (2D vs 3D), ultrasound route, parity, IOL indications, and geographic region. Publication bias was evaluated using Deeks’ funnel plot and Egger’s test [15]. A two-sided p-value <0.05 was considered statistically significant, except for the heterogeneity of Egger’s tests, where a p-value <0.1 was used. The statistical analyses were conducted using STATA software package, version 18.0. (Stata Corp, College Station, Texas, USA).
RESULTS
Study selection
Data were collected from three databases: EMBASE, MEDLINE, Scopus, and from Google Scholar. Studies from the reference lists of reviews, protocols, abstracts, and grey literature were also searched and selected. In total, 1396 eligible studies were included. Among these, 48 were excluded due to duplication. After screening the titles and abstracts, seven studies met the inclusion criteria and were incorporated into the final meta-analysis (Fig. 1).
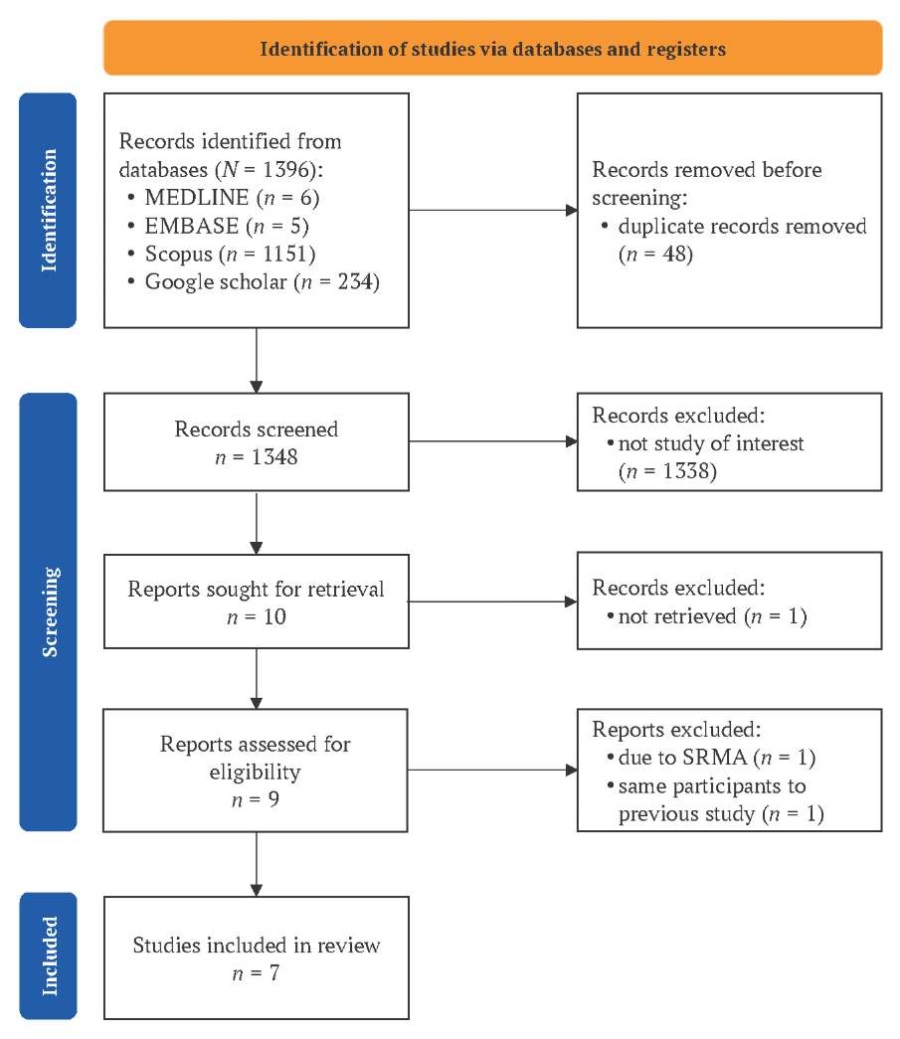
FIG. 1. PRISMA flowchart.
Note: SRMA – systematic review and meta-analysis.
Study characteristics
Seven prospective cohort studies [16–22] involving 534 pregnant women evaluated cervical volume via ultrasonography to predict successful IOL were included. Five studies [16][18–21] collected data primarily from Asia, whereas one study collected data from Africa [20] and one study from Europe [17]. One study [16] did not report the baseline characteristics of pregnant women. Sample sizes ranged from 36 to 126 participants per study (Table 1). Cervical volume was measured using two techniques: four studies employed three-dimensional ultrasonography using the Virtual Organ Computer-aided Analysis (VOCAL) software, while two studies utilized two-dimensional ultrasonography applying the cylinder volume formula (πR²h). Five studies used transvaginal ultrasonography, one study used translabial ultrasonography, and the ultrasound approach used in one study was not specified. Two studies reported a specific cervical volume cut-off value to predict successful IOL. The definitions of successful IOL varied across studies. Six studies defined successful IOL as VD, including four studies defined success as achieving VD within 24 hours and three studies defined success as achieving VD without a time limit. Two studies defined it as attaining the active phase of labor within 12 hours (Table 1).
Table 1. Key characteristics of included studies
Author, year | Sample size | VD/CD | Definition of successful IOL | Cervical volume cut-off value, cm³ | Ultrasound (type, name, method, route) |
Rovas, 2005a | 36 | 23/13 | VD 24 hours | NA | 3D, Voluson 730, VOCAL, TVS |
Rovas, 2005a | 36 | 32/4 | Achieved active phase of labor 12 hours | NA | 3D, Voluson 730, VOCAL, TVS |
Kim, 2010 | 41 | 30/11 | Achieved active phase of labor 12 hours | NA | 3D, Accuvix XQ, Medison, VOCAL, TVS |
Young, 2014 | 126 | 88/38 | VD | NA | NA |
Esin, 2016a | 38 | 29/9 | VD | NA | 3D, Volson, VOCAL, TLS |
Esin, 2016a | 29 | 20/9 | VD 24 hours | NA | 3D, Volson, VOCAL, TLS |
Athulathmudali, 2021 | 100 | 63/37 | VD 24 hours | 28.5 | 2D, Medison, cylinder volume formula, TVS |
İleri, 2023 | 125 | 93/32 | VD | NA | 3D, NA, VOCAL, TVS |
Elsheikh, 2024 | 68 | 37/31 | VD 24 hours | 27.0 | 2D, NA, 2D, Medison, cylinder volume formula, TVS |
Notes: a two different outcomes were accessed in the study.
CD – cesarean delivery (failed IOL); IOL – induction of labor; NA – not available; TLS – translabial ultrasound; TVS – transvaginal ultrasound; VD – vaginal delivery (successful IOL); VOCAL – Virtual Organ Computer-Aided Analysis; 2D – two-dimensional view; 3D – three-dimensional view.
The details of the patients’ characteristics and IOL methods are available for six eligible studies (Table 2). The mean age of participants across studies ranged from 25.7 to 33.0 years and the mean body mass index – from 24.0 to 30.5 kg/m². The mean gestational age varied between 37.7 and 42.3 weeks, and the mean estimated fetal weight – from 3174 to 3346 grams. Two studies enrolled only nulliparous women. Regarding the IOL methods, one study used only prostaglandin E1, four studies used prostaglandin E2, one study used prostaglandin E2 and a Foley’s catheter.
Table 2. Baseline characteristics of participants
Author, year | Mean age, year | Mean BMI, kg/m² | Nulliparous, % | Mean GA, weeks | Mean EFW, g | IOL method, % | Foley, % |
Rovas, 2005 | 33.0 | 30.5 | 47 | 42.3 | NA | PGE1 (100) | NA |
Kim, 2010 | 28.5 | 26.6 | 100 | 37.7 | 3174 | PGE2 (100) | NA |
Young, 2014 | NA | NA | 100 | NA | NA | NA | NA |
Esin, 2016 | 25.7 | 30.4 | 50 | 41.0 | 3346 | PGE2 (69.6) | 30.4 |
Athulathmudali, 2021 | 28.4 | 24.0 | 71 | 39.9 | 3071 | PGE2 (100) | NA |
İleri, 2023 | 27.6 | 28.7 | 50.4 | 38.8 | 3179 | PGE2 (100) | NA |
Elsheikh, 2024 | 25.7 | 26.9 | NA | 38.9 | 3181 | PGE2 (100) | NA |
Note: BMI – body mass index; EFW – estimated fetal weight; GA – gestational age; IOL – induction of labor; NA – not available; PGE1 – prostaglandin E1; PGE2 – prostaglandin E2.
Risk of bias in studies
Risk of bias assessment could not be performed in one study [16] due to unavailability of the full-text article. Among the remaining studies, four studies [17][20–22] were considered low risk of bias (Fig. 2). Whereas two studies were regarded as high risk of bias: one study [18] raised concerns in the domains of ascertainment of exposure, follow-up period adequacy, and comparability, while another study [20] identified a high risk in the representativeness of the exposed cohort, ascertainment of exposure, and comparability.
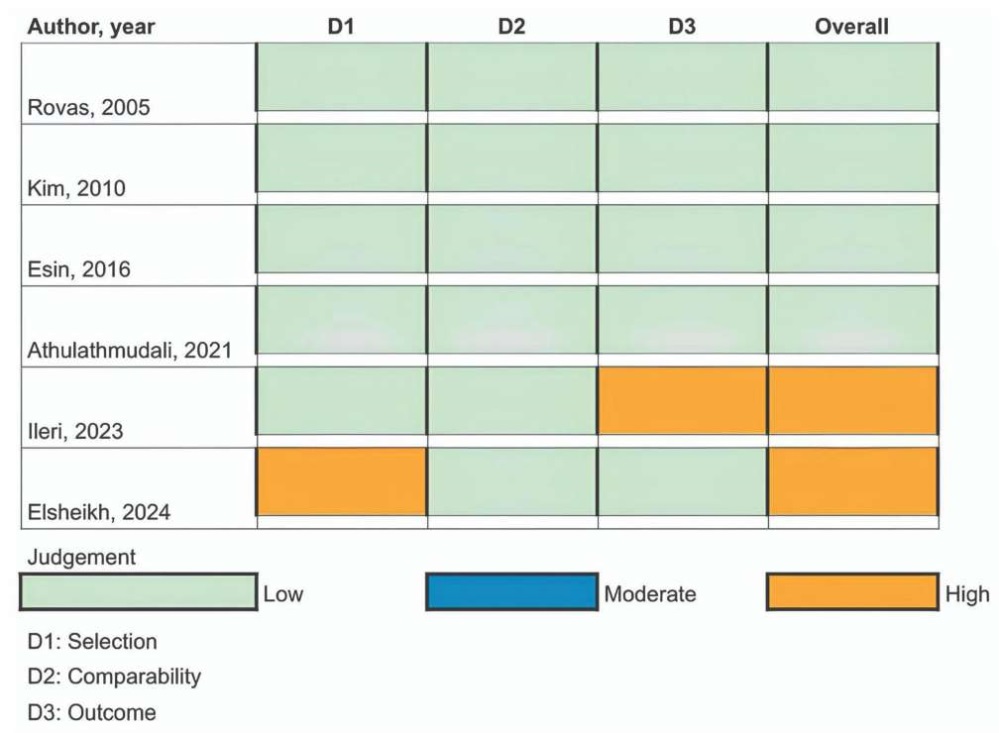
FIG. 2. Traffic light plot for cohort studies using the modified Newcastle–Ottawa scale.
Note: D1 – selection domain; D2 – comparability domain; D3 – outcome domain.
Indication for induction of labor
Six studies reported the indications for IOL (Table 3). Among IOL, pregnancy-induced hypertension demonstrated a median prevalence of 11.45%, gestational diabetes mellitus – 8.8%, fetal growth restriction – 13.90%, oligohydramnios – 18.76%, post-term pregnancy – 41.30%, premature ruptured of membrane – 28.1%, large for gestational age – 18.6%, non-reassuring fetal status – 11.2%, maternal condition – 19.5%.
Table 3. Indication for induction of labor of included studies
Author, year | PIH, % | GDM, % | FGR, % | OHA, % | PTP, % | PROM, % | LGA, % | NRFS, % | MC, % |
Rovas, 2005 | 7.9 | NA | 7.9 | 68.4 | 7.9 | NA | 7.9 | NA | NA |
Kim, 2010 | 14.6 | 9.8 | 19.5 | 4.9 | NA | NA | 29.3 | NA | 19.5 |
Young, 2014 | NA | NA | NA | NA | 100 | NA | NA | NA | NA |
Esin, 2016 | 8.3 | NA | 8.3 | 18.8 | 64.6 | NA | NA | NA | NA |
Athulathmudali, 2021 | 6.0 | 33.0 | NA | NA | 61.0 | NA | NA | NA | NA |
İleri, 2023 | 20.0 | 7.2 | 22.4 | 12.0 | 21.6 | NA | NA | 11.2 | 4.8 |
Elsheikh, 2024 | 17.2 | 7.8 | NA | 6.3 | 20.3 | 28.1 | NA | NA | 20.3 |
Note: FGR – fetal growth restriction; GDM – gestational diabetes mellitus; LGA – large for gestational age; MC – maternal condition; NA – not available; NRFS – non-reassuring fetal status; OHA – oligohydramnios; PIH – pregnancy-induced hypertension; PROM – premature ruptured of membrane; PTP – post-term pregnancy.
Maternal outcomes
Cervical volume cut-off value and successful VD within 24 hours
Two studies involving 168 pregnant women evaluated cervical volume using different cutoff values of 27 cm³ and 28.5 cm³. Pooled analysis demonstrated positive association between lower cervical volume and successful VD within 24 hours (OR 7.19; 95% CI: 3.31 to 15.64; τ² = 0.00; I² = 0%; 95% predictive interval (approximate, normal-quantile due to only two studies): 3.31 to 15.64; Fig. 3A).
Mean cervical volume and successful VD and CD
Five studies involving 422 pregnant women reported cervical volume without specific cut-off values. Notably, Esin et al. [19] reported data for two predefined outcome definitions: VD without a specified timeframe and VD within 24 hours, which were analyzed separately. The pooled analysis showed no statistically significant difference between successful and failed IOL (MD –1.32 cm³; 95% CI: –8.37 to 5.72; I² = 89.8%; Fig. 3B). The mean cervical volume in successful IOL ranged from 23.99 with 6.04 cm³ to 44.17 with 8.66 cm³, whereas in failed IOL – from 30.1 with 14.7 cm³ to 48.07 with 11.34 cm³. Two studies found a significant difference in cervical volume between successful and failed IOL: 36.21 with 9.62 cm³ vs. 48.07 with 11.34 cm³ (p < 0.01) [17] and 23.99 with 6.04 cm³ vs. 29.80 with 7.38 cm³ (p = 0.02) [22], respectively.
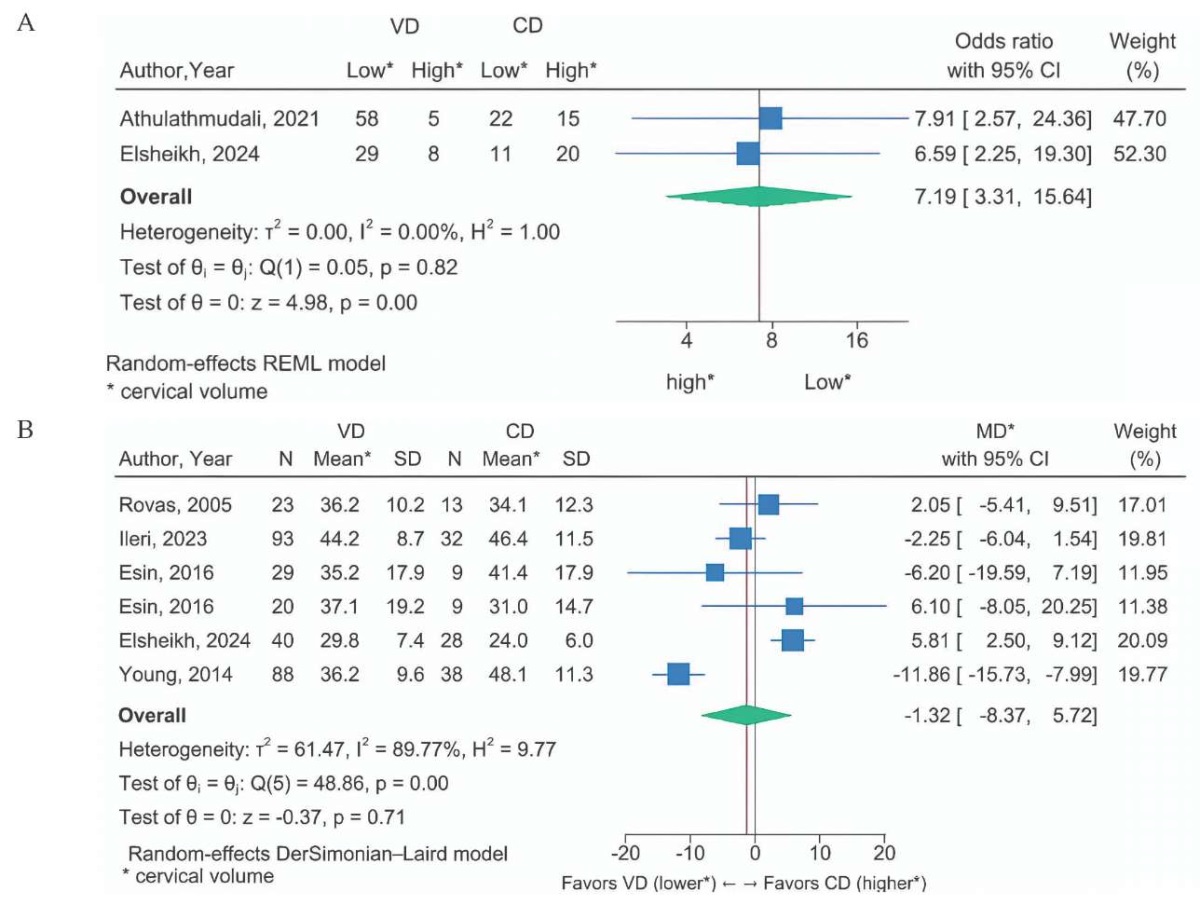
FIG. 3. Forest plots showing weighted effect.
A. Cervical volume cut-off value.
B. Mean cervical volume.
Notes: * cervical volume.
CD – cesarean delivery; CI – confidence interval; MD – mean difference; VD – vaginal delivery.
Subgroup analysis
The sources of heterogeneity were explored among the studies using subgroup analysis. Three studies involving 289 pregnant women defined successful IOL as VD without a timeframe. The pooled analysis showed that women with successful VD had a lower mean cervical volume (MD –6.88 cm³; 95% CI: −14.6 to 0.83 cm³; I² = 83.5%) without a statistically significant difference (Fig. 4A). Exclusion of the outlier study by Young et al. [16] reduced heterogeneity to zero (I² = 0%) but did not change the non-significant difference between groups (MD –2.54 cm³; 95% CI: –6.19 to 1.11; Fig. 4B).
Three studies involving 133 pregnant women defined a successful IOL as a VD within 24 hours. The pooled analysis demonstrated no significant difference between the two groups (MD 5.23 cm³; 95% CI: 2.27 to 8.19; I² = 0; Fig. 4C)
Two studies involving 77 pregnant women defined successful IOL as actively going into labor within 12 hours. Pregnant women who achieved the active phase of labor had a lower mean cervical volume compared with those who did not (MD –5.73 cm³; 95% CI: –10.64 to –0.81; I² = 0%, 95% predictive interval (approximate, normal-quantile due to only two studies): −10.64 to −0.81; Fig. 4D).
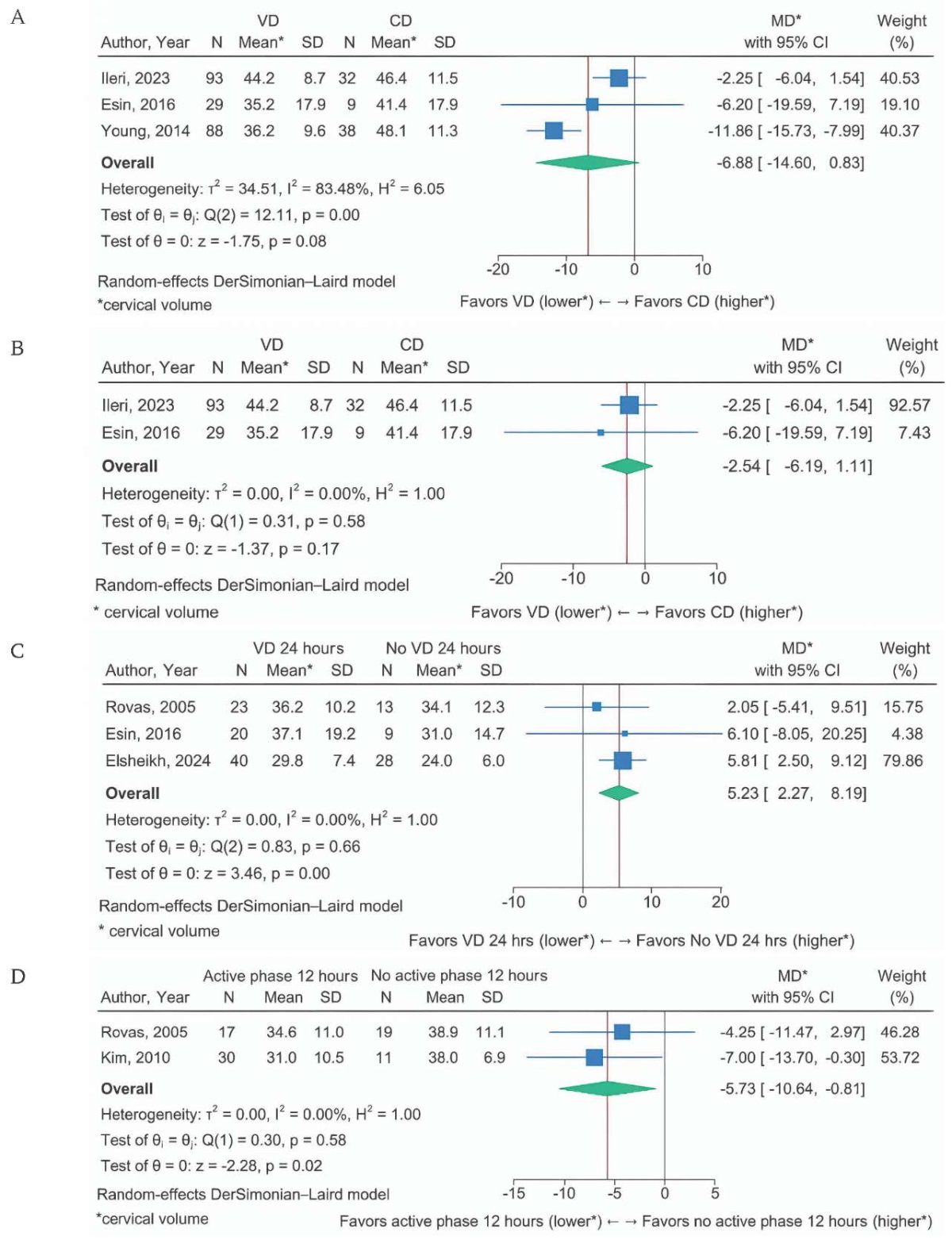
FIG. 4. Forest plots showing subgroup analysis.
A. Outcome without timeframe.
B. Outcome without timeframe (sensitivity analysis).
C. Outcome within 24 hours.
D. Outcome within 12 hours.
Notes: * cervical volume.
CD – cesarean delivery; CI – confidence interval; MD – mean difference; VD – vaginal delivery.
Publication bias
Visual inspection of the contour-enhanced funnel plot demonstrated no substantial asymmetry (Fig. 5). Egger’s regression test confirmed the absence of small-study effects (coefficient = 0.50, standard error = 1.75, p = 0.78), indicating no evidence of publication bias.
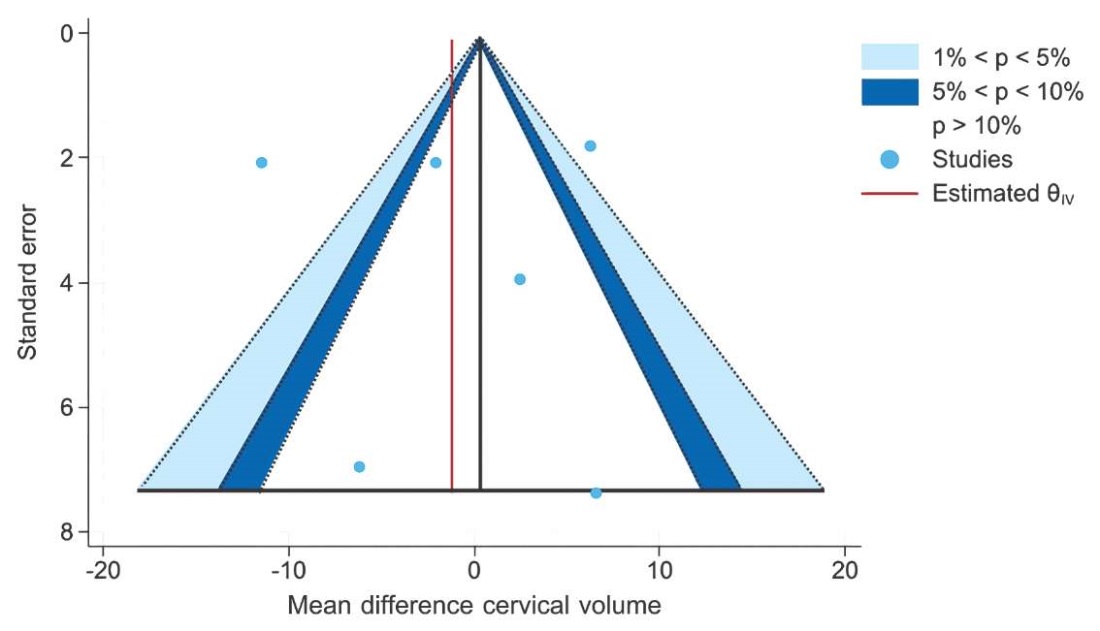
FIG. 5. Funnel plot for a meta-analysis of 7 cohort studies.
DISCUSSION
This systematic review and meta-analysis evaluate the association between cervical volume and successful IOL. The aggregated data from seven prospective cohort studies suggest that cervical volume, as an objective sonographic parameter, may have a clinically meaningful predictive value in estimating the probability of successful IOL. Specifically, pooled results demonstrate that lower cervical volume cutoff values (less than 27 to 28.5 cm³) are strongly associated with VD within 24 hours (OR 7.19), although the estimate has wide precision (95% CI: 3.31–15.64).
When compared with the Bishop score for predicting successful IOL, reported ORs for achieving VD within a specified timeframe ranged from 2.15 to 4.22 [6]. Other ultrasonographic cervical parameters demonstrated a similar direction of association. For example, cervical length with cut-off values of 25 mm, 32 mm, and 40 mm yielded ORs of approximately 5.52, 7.88, and 7.78, respectively, for predicting VD within 24 hours [10]. The presence of cervical wedging was associated with an OR of approximately 2.14 [10], cervical elastography with an OR of 2.97 [8], and the uterocervical angle with an OR of about 4.33 for predicting successful IOL [7]. Based on these findings, cervical volume appears to have a stronger association with successful IOL than other ultrasonographic cervical parameters. However, only two studies [20][22] provided data on cervical volume, which limits the robustness of this conclusion. In addition, this analysis did not directly compare cervical volume with other ultrasonographic cervical parameters within the same study populations. Variations in the definitions of outcomes, especially differences in the timeframe from induction to delivery, may further reduce the comparability of results across studies.
This review evaluated the criteria for defining the timing of successful IOL as a notable outcome. Studies of cervical volume without cut-off values underwent subgroup analysis for specified versus unspecified time in the VD outcome. Smaller cervical volume was associated with successful VD and the achievement of an active phase within 12 hours. However, the results indicated the opposite for successful VD without timeframe, where larger cervical volume was associated with VD within 24 hours. Therefore, the reliability of these findings may be limited due to the small number of included studies and the possibility that the timeframe used to define successful IOL is overly restrictive. Clinicians evaluating the probability of VD should interpret these results cautiously, as strict time-based definitions, such as requiring VD within 24 hours, may reduce the applicability of the study’s results.
Both VD and achievement of the active phase of labor showed a high level of heterogeneity. A subgroup analysis was performed to explore the sources of heterogeneity in the included studies based on the varying definitions of outcomes [23]. When subgrouping by VD without timeframe, I² decreased, indicating that one of the sources of heterogeneity was the definition of outcomes within a timeframe. Therefore, the interpretation of the results caused inconsistencies. Additionally, a sensitivity analysis for the outcome of VD within 24 hours was performed by excluding one study [16]; this method could clarify the source of heterogeneity when I² was reduced. However, other factors including maternal age, body mass index, gestation age, nulliparity, type of ultrasound, methods of IOL, and indication for IOL, might also have contributed to heterogeneity, because I² was not reduced after analysis of these variables.
Furthermore, cervical volume measurement techniques, using either 2D or 3D, influenced the variability of the results in this study. Subgroup analysis of studies employing 2D ultrasonography showed lower heterogeneity than when 2D and 3D were combined. Although 2D cervical volume measurement is simpler and more accessible, it assumes a uniform cylindrical shape of the cervix, which may not precisely reflect cervical anatomy, whereas the 3D technique offers potentially more accurate volume estimation. However, this technique is operator-dependent and requires specific skills and experience, which may contribute to inter-observer variability [24].
For risk of bias assessment, although most observational studies were considered to have a low risk, careful interpretation is still needed, particularly regarding potential issues with cohort comparability and outcome measurements. In terms of publication bias, although Egger’s test did not demonstrate a significant small-study effect and the funnel plot appeared generally symmetrical, the ability to detect asymmetry is limited due to the small number of included studies. Therefore, any conclusions that are drawn regarding publication bias should be made cautiously. While contour-enhanced funnel plots help visualize study distribution, any observed asymmetry may reflect true heterogeneity, methodological variation, or selective publication.
This study assessed specific outcomes, including successful VD and achievement of the active phase of labor, and analyzed subgroups by specified versus non-specified timeframe, which provided a more precise context for interpretation and reduced heterogeneity. Although the association among included studies was similar for VD without a timeframe, heterogeneity was substantial, with one study contributing a markedly high MD. A sensitivity analysis was therefore conducted to explore potential sources of heterogeneity. The results indicated that pregnant women with successful VD had a smaller cervical volume than those without. Sources of heterogeneity were further explored based on different clinical definitions to improve consistency. Additionally, inclusion was not restricted to published papers. Other relevant sources were considered to make the evidence base as diverse and comprehensive as possible, reduce the publication bias, and to make sure the findings are as valid as can be.
Limitations of the study
This meta-analysis has several limitations. First, it included only seven studies, rendering it statistically less compelling and reducing the confidence in the pooled estimates. Second, most studies were conducted in Asia, with only one each from Europe and Africa. This geographic imbalance may reflect differences in clinical practice and available resources, which could affect the generalizability of our findings. Third, cervical volume was measured using different ultrasound modalities (2D vs 3D). Currently, no standard method exists, and thus there is an element of measurement variability. Fourth, some studies had a high risk of bias, especially in exposure ascertainment, follow-up adequacy, and comparability. One study could not be assessed due to the lack of access to the full-text. Fifth, conflicting findings were observed regarding cervical volume and VD, possibly due to the timeframe used (within 24 hours vs any time), which may influence the interpretation. Lastly, substantial heterogeneity was present, likely exacerbated by the small number of included studies. All of these factors should be taken into consideration when interpreting the results. Of course, further research is needed to confirm all these findings.
Directions for further research
This study supports the potential role of cervical volume in predicting successful IOL, but several aspects require further investigation. First, standardized measurement methods should be developed to reduce variability in techniques (e.g., 2D vs 3D, use of VOCAL vs cylinder volume formula, and ultrasound approach), which can affect measurement reliability. Second, studies with larger and more diverse populations are needed to improve generalizability. Third, combining cervical volume with other clinical or sonographic parameters may enhance clinical utility. Finally, research should evaluate the clinical value of cervical volume in routine pre-induction assessments.
CONCLUSIONS
Cervical volume has significant potential as a parameter for predicting successful IOL in decision support frameworks in obstetrics. While some studies report smaller cervical volume being associated with better IOL outcomes, subgroup findings remain inconclusive. Ultrasonography to determine cervical volume can be combined with other clinical maternal and fetal parameters to enhance decision support systems and revolutionize delivery care in obstetrics. Further research using standardized cervical volume measurement methods, larger sample sizes, broader geographic representation, and analyses of pregnant women of the same parity may improve the precision of ultrasonographic cervical volume as a predictor of successful IOL.
AUTHOR CONTRIBUTIONS
Potsanop Kassayanan and Monchai Suntipap developed the concept and design of the study, as well as analyzed and interpreted the data. Potsanop Kassayanan, Prame Chantabal and Monchai Suntipap collected the primary data. Monchai Suntipap performed the statistical analysis. Potsanop Kassayanan, Kasidis Nontaprom, Switta Thanasantumrongsak and Monchai Suntipap drafted the manuscript and took part in the critical revision of the manuscript. All the authors approved the final version of the article.
ВКЛАД АВТОРОВ
П. Кассаянан и М. Сунтипап разработали концепцию и дизайн исследования, участвовали в анализе и интерпретации данных. П. Кассаянан, П. Чантабал и М. Сунтипап участвовали в сборе первичных данных. М. Сунтипап проводил статистический анализ. П. Кассаянан, К. Нонтапром, С. Танасантумронгсак и М. Сунтипап участвовали в подготовке текста и провели критический анализ рукописи. Все авторы одобрили окончательную версию статьи.
Ethics statements. The study was registered in PROSPERO under the registration number CRD42024579753.
Data availability. The data confirming the findings of this study are available from the authors upon reasonable request. Data and statistical methods used in the article were examined by a professional biostatistician on the Sechenov Medical Journal editorial staff.
Conflict of interest. The authors declare that there is no conflict of interests.
Financing. The study had no sponsorship (own resources).
Соответствие принципам этики. Исследование зарегистрировано на PROSPERO, регистрационный номер CRD42024579753.
Доступ к данным исследования. Данные, подтверждающие выводы этого исследования, можно получить у авторов по обоснованному запросу. Данные и статистические методы, представленные в статье, прошли статистическое рецензирование редактором журнала – сертифицированным специалистом по биостатистике.
Конфликт интересов. Авторы заявляют об отсутствии конфликта интересов.
Финансирование. Исследование не имело спонсорской поддержки (собственные ресурсы).
1. WHO recommendations on induction of labour, at or beyond term. World Health Organization; 2022. p 43 (access date: 01.11.2024).
2. Kassayanan P., Chantabal P., Suntipap, M. Ultrasonography cervical volume as a predictor of successful induction of labor in pregnant women with induction of labor, A systematic review and Meta-analysis. Procedia of Multidisciplinary Research. 2024. 2(10): 99.
3. Collaboration for environmental evidence. Guidelines and standards for evidence synthesis in environmental management. Pullin AS, GK Frampton, B Livoreil & G Petrokofsky, editors. 2022. http://www.environmentalevidence.org/information-for-authors (access date: 31.07.2025).
4. Wells GA, Shea B, O’Connell D, Peterson J, Welch V, Losos M, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. 2000. https://www.ohri.ca/programs/clinical_epidemiology/oxford.asp (access date: 04.11.2024).
References
1. ACOG Practice Bulletin No. 107: Induction of labor. Obstet Gynecol. 2009 Aug; 114(2 Pt 1): 386–397. https://doi.org/10.1097/AOG.0b013e3181b48ef5. PMID: 19623003
2. Seyb S.T., Berka R.J., Socol M.L., Dooley S.L. Risk of cesarean delivery with elective induction of labor at term in nulliparous women. Obstet Gynecol. 1999 Oct; 94(4): 600–607. https://doi.org/10.1016/s0029-7844(99)00377-4. PMID: 10511367
3. Erekson E.A., Myles T.D. Risks for chorioamnionitis with both induction and augmentation of labor. Obstetrics & Gynecology. 2006; 107(4): 32S–33S. https://doi.org/10.1097/00006250-200604001-00075
4. Rossi A.C., Prefumo F. Pregnancy outcomes of induced labor in women with previous cesarean section: a systematic review and meta-analysis. Arch Gynecol Obstet. 2015 Feb; 291(2): 273–280. https://doi.org/10.1007/s00404-014-3444-9. Epub 2014 Sep 2. PMID: 25178187
5. Kolkman D.G., Verhoeven C.J., Brinkhorst S.J., et al. The Bishop score as a predictor of labor induction success: a systematic review. Am J Perinatol. 2013 Sep; 30(8): 625–630. https://doi.org/10.1055/s-0032-1331024. Epub 2013 Jan 2. PMID: 23283806
6. Teixeira C., Lunet N., Rodrigues T., Barros H. The Bishop Score as a determinant of labour induction success: a systematic review and meta-analysis. Arch Gynecol Obstet. 2012 Sep; 286(3): 739– 753. https://doi.org/10.1007/s00404-012-2341-3. Epub 2012 May 1. PMID: 22546948
7. Yang S.W., Kim S.Y., Hwang H.S., et al. The uterocervical angle combined with Bishop score as a predictor for successful induction of labor in term vaginal delivery. J Clin Med. 2021 May 10; 10(9): 2033. https://doi.org/10.3390/jcm10092033. PMID: 34068513
8. Londero A.P., Schmitz R., Bertozzi S., et al. Diagnostic accuracy of cervical elastography in predicting labor induction success: a systematic review and meta-analysis. J Perinat Med. 2016 Mar; 44(2): 167–178. https://doi.org/10.1515/jpm-2015-0035. PMID: 26011923
9. Shi Q., Wang Q., Tian S., et al. Assessment of different sonographic cervical measures to predict labor induction outcomes: a systematic review and meta-analysis. Quant Imaging Med Surg. 2023; 13(12): 8462–8477. https://doi.org/10.21037/qims-23-507. PMID: 38106269
10. Verhoeven C.J., Opmeer B.C., Oei S.G., et al. Transvaginal sonographic assessment of cervical length and wedging for predicting outcome of labor induction at term: a systematic review and metaanalysis. Ultrasound Obstet Gynecol. 2013 Nov; 42(5): 500–508. https://doi.org/10.1002/uog.12467. PMID: 23533137
11. Al-Adwy A.M., Sobh S.M., Belal D.S., et al. Diagnostic accuracy of posterior cervical angle and cervical length in the prediction of successful induction of labor. Int J Gynaecol Obstet. 2018 Apr; 141(1): 102–107. https://doi.org/10.1002/ijgo.12425. Epub 2018 Jan 18. PMID: 29224196
12. Page M.J., McKenzie J.E., Bossuyt P.M., et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021 Mar 29; 372: n71. https://doi.org/10.1136/bmj.n71. PMID: 33782057
13. Wan X., Wang W., Liu J., Tong T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol. 2014 Dec 19; 14: 135. https://doi.org/10.1186/1471-2288-14-135. PMID: 25524443
14. Higgins J.P., Thompson S.G., Deeks J.J., Altman D.G. Measuring inconsistency in meta-analyses. BMJ. 2003 Sep 6; 327(7414): 557–560. https://doi.org/10.1136/bmj.327.7414.557. PMID: 12958120
15. Egger M., Davey Smith G., Schneider M., Minder C. Bias in metaanalysis detected by a simple, graphicaltest. BMJ. 1997 Sep 13; 315(7109): 629–634. https://doi.org/10.1136/bmj.315.7109.629. PMID: 9310563
16. Young L., Ki Cheol K., Ji-sun W., et al. P 17.13: Cervical volume is a good predictor of successful labour induction. Ultrasound in Obstetrics & Gynecology. 2014; 44(S1): 289. https://doi.org/10.1002/uog.14346
17. Rovas L., Sladkevicius P., Strobel E., Valentin L. Threedimensional power Doppler ultrasound assessment of the cervix for the prediction of successful induction of labor with prostaglandin in prolonged pregnancy. J Ultrasound Med. 2005 Jul; 24(7): 933–939. https://doi.org/10.7863/jum.2005.24.7.933. PMID: 15972707
18. İleri A., Yıldırım Karaca S., Gölbaşı H., et al. Diagnostic accuracy of pre-induction cervical elastography, volume, length, and uterocervical angle for the prediction of successful induction of labor with dinoprostone. Arch Gynecol Obstet. 2023 Oct; 308(4): 1301–1311. https://doi.org/10.1007/s00404-023-07076-8. Epub 2023 May 21. PMID: 37210702
19. Esin S., Yirci B., Yalvac S., Kandemir O. Use of translabial threedimensional power Doppler ultrasound for cervical assessment before labor induction. J Perinat Med. 2017 Jul 26; 45(5): 559– 564. https://doi.org/10.1515/jpm-2016-0206. PMID: 27977408
20. Elsheikh M., Sadek M., Swidan E., Ahmed E. Cervical volume assessment to predict the result of induction of labor: a prospective observational study. Benha Journal of Applied Sciences. 2024; 9(2): 7–15. https://doi.org/10.21608/bjas.2024.268427.1323
21. Kim Y.H., Kim J.W., Kim C.H., et al. Evaluation of length, volume and gray-scale histogram of the cervix as predictors of successful induction. Korean Journal of Obstetrics and Gynecology. 2010; 53(5): 389–395. https://doi.org/10.5468/kjog.2010.53.5.389
22. Athulathmudali S.R., Patabendige M., Chandrasinghe S.K., De Silva P.H.P. Transvaginal two-dimensional ultrasound measurement of cervical volume to predict the outcome of the induction of labour: a prospective observational study. BMC Pregnancy Childbirth. 2021 Jun 22; 21(1): 433. https://doi.org/10.1186/s12884-021-03929-9. PMID: 34158010
23. Suvorov A.Yu., Latushkina I.V., Gulyaeva K.A., et al. Basic aspects of meta-analysis. Part 1. Sechenov Medical Journal. 2023; 14(1): 4–14. https://doi.org/10.47093/2218-7332.2023.14.1.4-14. EDN: RORJSI
24. Basgul A., Kavak Z.N., Bakirci N., Gokaslan H. Intra- and interobserver agreement on cervical volume and flow indices during pregnancy using transvaginal 3-dimensional ultrasonography and Doppler angiography. Int J Fertil Womens Med. 2006 Nov-Dec; 51(6): 256–261. PMID: 17566567
About the Authors
P. KassayananThailand
Potsanop Kassayanan, student, Faculty of Medicine
114, Sukhumvit 23 str., Wattana District, Bangkok, 10110
K. Nontaprom
Thailand
Kasidis Nontaprom, student, Faculty of Medicine
114, Sukhumvit 23 str., Wattana District, Bangkok, 10110
P. Chantabal
Thailand
Prame Chantabal, MD, gynecologist, Department of Obstetrics and Gynecology
30, M.7 Khlong Hok, Khlong Luang District, Pathum Thani, 12120
S. Thanasantumrongsak
Thailand
Switta Thanasantumrongsak, student, Faculty of Medicine
114, Sukhumvit 23 str., Wattana District, Bangkok, 10110
M. Suntipap
Thailand
Monchai Suntipap, MD, MSc, lecturer, doctor, Department of Obstetrics and Gynecology
114, Sukhumvit 23 str., Wattana District, Bangkok, 10110
Supplementary files

|
1. Supplementary materials | |
| Subject | ||
| Type | Исследовательские инструменты | |
Download
(833KB)
|
Indexing metadata ▾ | |

|
2. PRISMA checklist | |
| Subject | ||
| Type | Research Instrument | |
Download
(159KB)
|
Indexing metadata ▾ | |

|
3. 1223-PRISMA checklist | |
| Subject | ||
| Type | Исследовательские инструменты | |
Download
(176KB)
|
Indexing metadata ▾ | |
Review
Sechenov Medical Journal. Editor's checklist for this article you can find here.
Название / Title | Объем шейки матки, оцененный по ультразвуковому исследованию, как предиктор успешной родовой деятельности: систематический обзор и метаанализ / Ultrasonography cervical volume as a predictor of successful induction of labor: a systematic review and meta-analysis |
Раздел / Section
| АКУШЕРСТВО И ГИНЕКОЛОГИЯ / ОBSTETRICS AND GYNECOLOGY |
Тип / Article | Систематический обзор / Systematic review |
Номер / Number | 1223
|
Страна/территория / Country/Territory of origin | Таиланд / Thailand |
Язык / Language | Английский / English
|
Источник / Manuscript source | Инициативная рукопись / Unsolicited manuscript |
Дата поступления / Received | 30.04.2025 |
Тип рецензирования / Type ofpeer-review | Двойное слепое / Double blind |
Язык рецензирования / Peer-review language | Английский / English |
РЕЦЕНЗЕНТ А / REVIEWER A
Инициалы / Initials | 1223_А
|
Научная степень / Scientific degree | Кандидат медицинских наук / Cand. of Sci. (Medicine)
|
Страна/территория / Country/Territory | Россия / Russia
|
Дата рецензирования / Date of peer-review | 30.06.2025
|
Число раундов рецензирования / Number of peer-review rounds | 2 |
Финальное решение / Final decision | принять к публикации / accept
|
ПЕРВЫЙ РАУНД РЕЦЕНЗИРОВАНИЯ / FIRST ROUND OF PEER-REVIEW
Scientific quality: Grade B: Good
Language quality: Grade B (Minor language polishing)
Re-review: Yes
This meta-analysis addresses a clinically important question: identifying predictors of successful induction of labor to reduce maternal and fetal risks. The study design is robust, adhering to PRISMA guidelines and PROSPERO registration, with a comprehensive search across databases. The inclusion of seven prospective cohort studies and subgroup analysesfor varying definitions of success strengthens its relevance to clinical decision-making.
Comments
1) association between cervical volume and IOL success reverses direction depending on outcome timing (smaller volume linked to success in some subgroups, larger in others), creating conflicting conclusions. This issue should be thoroughly addressed in limitations and discussion.
2) Results of Deeks’ funnel plot and Egger’s test are mentioned but not reported, limiting assessment of potential bias.
3) High heterogeneity (Heterogeneity Index up to 89%) and inclusion of only seven studies weaken confidence in pooled estimates. Authors encouraged to address this issue in limitations.
4) Two studies rated as high risk, and geographic diversity is limited (most from Asia), raising concerns about generalizability.
5) The abstract/conclusion emphasizes smaller cervical volume as beneficial despite conflicting subgroup results.
Recommendation after the first round of peer-review: major revision and re-review.
ВТОРОЙ РАУНД РЕЦЕНЗИРОВАНИЯ /SECOND ROUND OF PEER-REVIEW
All comments have been addressed by authors.
РЕЦЕНЗЕНТ B / REVIEWER B
Инициалы / Initials | 1223_В
|
Научная степень / Scientific degree | Кандидат медицинских наук / Cand. of Sci. (Medicine)
|
Страна/территория / Country/Territory | Россия / Russia
|
Дата рецензирования / Date of peer-review | 30.05.2025 |
Число раундов рецензирования / Number of peer-review rounds | 1 |
Финальное решение / Final decision | Принять к публикации после небольшой доработки/ Minor revision
|
ПЕРВЫЙ РАУНД РЕЦЕНЗИРОВАНИЯ / FIRST ROUND OF PEER-REVIEW
Scientific quality: Grade B: Good
Language quality: Grade B (Minor language polishing)
Re-review: No
The authors conducted a high-quality systematic review and meta-analysis. Its methodology and composition raises only a few minor issues:
Q1. Line 429. The sentence “The modified NOS evaluated six studies but limited data for
diagnostic perfor-mance evaluation using the QUADAS-2 tool” is not quite clear. The authors are suggested to rephrase it and to detail why this tool was not applicable.
Q2. The authors may consider re-structuring the manuscript: risk of bias seems to be more appropriate after the section “Characteristics of included studies”. Table 4 may be moved to supplementary material as this data is shown at Figure 3.
РЕКОМЕНДАЦИИ НАУЧНЫХ РЕДАКТОРОВ ЖУРНАЛА / RECOMMENDATIONS
OF THE SCIENTIFIC EDITORS OF THE JOURNAL
Main text
- To ensure that the main findings, clinical relevance and novelty of the study are clearly and concisely communicated to the reader, it is necessary to add three to five key highlights of the paper. These highlights improve the article’s visibility and facilitate rapid appraisal by clinicians and researchers conducting focused literature searches.
- A traffic light plot for the risk-of-bias assessment should be provided, as this visual representation allows readers and reviewers to easily evaluate the methodological quality of the included studies. This is an essential element of high-quality systematic reviews, contributing to greater transparency and reproducibility of the findings.
- Funnel plots and the results of Egger’s test must be included to assess potential publication bias. These analyses strengthen the credibility and robustness of the meta-analysis, demonstrating that the authors have critically evaluated the risk of systematic distortion in the available evidence.
Technical requirements
- To ensure transparency, accountability, and accurate indexation in scientific databases, including PubMed, it is necessary to provide full information for all authors, including academic degree and title (if applicable), position, and place of work (or study). Providing complete author details also ensures compliance with international publication standards, including the recommendations of the International Committee of Medical Journal Editors (ICMJE).
- Submitting all figures as separate, high-quality files ensures clear and accurate visualization in both the online and print versions of the journal. Low-resolution or poor-quality images may compromise readability, reduce the scientific value of the article and affect its suitability for indexing negatively.
- It is essential to provide Figure 1 in an editable format (e.g. PPTX) rather than as a screenshot to ensure professional layout and consistent formatting. Editable files allow technical adjustments to be made during the production process, whereas screenshots cannot be modified without loss of quality.
- The reference list must be formatted in accordance with Vancouver style to ensure consistency, a professional presentation, accurate database indexing and compliance with the journal's editorial policy and international standards.
- Providing the DOI and PMID (if available) for each reference is essential to facilitate accurate indexing in international databases, enabling readers to locate the original sources efficiently, a key requirement of high-quality scientific publishing.
References
- To reflect the current state of knowledge and ensure that the review is based on the most up-to-date and relevant evidence, it is necessary to add recent studies to the reference list, with the majority of references preferably published within the last five years.
- As most of the included studies originate from Asia, it is important to clarify whether this topic has been investigated in other regions. The geographic diversity of the included studies should be increased, or a clear justification for the current regional focus should be provided. Overrepresentation of a single region may introduce geographical or population bias, limiting the generalizability of the conclusions. Addressing this issue would significantly strengthen the study's scientific validity.
JATS XML