EDITORIAL
Dear colleagues, In the end of 2019, the world faced a new threat — COVID-19 caused by the new coronavirus SARS-CoV-2. On March 11, 2020, the World Health Organization declared the beginning of the pandemic. In Russia, the maximum number of cases was registered in Moscow: as of the end of September 2020, their number exceeded 300 thousand. Since the 19th of March 2020, a Federal Remote Advisory Center for Anesthesiology and Resuscitation for Adults has been functioning at Sechenov University, a leading medical HEI in Russia. Highly qualified specialists consult 24/7 the most severe COVID-19 patients from all regions of the Russian Federation. 2,919 staff members of Sechenov University participated in treatment of 6,009 COVID-19 patients on the bases of four University hospitals during the period from April 8 till August 10, 2020. Considering the vast experience in the diagnosis and treatment of COVID-19 accumulated by the University and our colleagues during the pandemic, a decision has been made to devote one of the Sechenov Medical Journal issues to this problem. The issue covers a wide range of COVID-19 associated problems: the pathogenesis of the disease, diagnostic capabilities of ultrasound examination of lungs, treatment features for oncology patients, cardiovascular safety assessment of hydroxychloroquine combined with azithromycin, effectiveness of corticosteroids, features of damage to the organ of vision, legislative regulation of health protection in an epidemic. We very much hope, the information in this issue will help fighting against this dangerous infection!
COVID-19
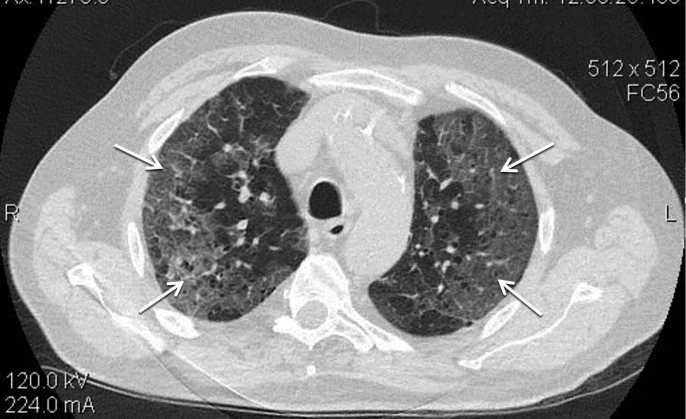
Lung ultrasound demonstrates a high diagnostic value in the assessment of lung diseases.
Aim. To determine the diagnostic accuracy of lung ultrasound compared to chest computed tomography (CT) in the diagnosis of lung changes in COVID-19.
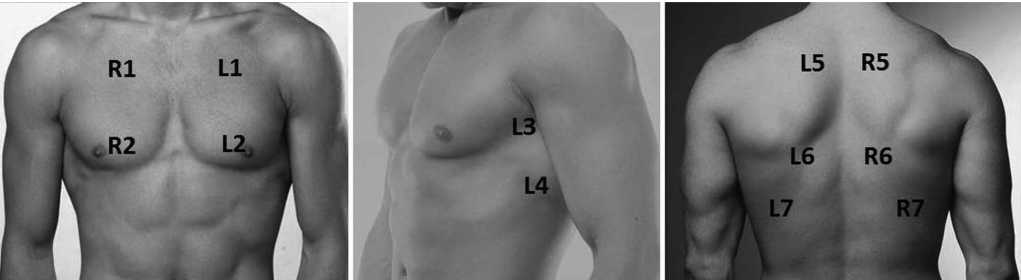
Materials and methods. The retrospective study included 45 patients (28 men) aged 37 to 90 years who underwent polypositional lung ultrasound with an assessment of 14 zones. The study compared lung echograms with chest CT data in assessing the prevalence of the process and the nature of structural changes. The diagnostic accuracy, sensitivity, and specificity of lung ultrasound in comparison with CT scans were determined, 95% confidence intervals (CI) were calculated.
Results. In 44 patients (98%), CT revealed pathological changes with subpleural localization in both lungs. Of these, in 30 cases, the inflammation was limited only to the subpleural parts, and in 14 cases, the changes spread to the basal parts of the lungs, while ultrasound revealed changes at the depth of the lesion no more than 4 cm. The lesion of 10–11 zones according to lung ultrasound corresponds to CT 1–2 degrees, the lesion of 13–14 zones — CT 3–4 degrees. The sensitivity of ultrasound to detect lung changes of various types was ≥ 92%. The highest sensitivity of 97.9% (95% CI: 92.8–99.8%) was determined for small consolidations on the background of interstitial changes (degree 1A+, 1B+), which corresponded to “crazy-paving” pattern on CT. The specificity depended on the nature of the changes and varied from 46.7 to 70.0%. Diagnostic accuracy was ≥ 81%, the maximum values of 90.6% (95% CI: 85.6–94.2%) were obtained for moderate interstitial changes (grade 1A) corresponding to ground-glass opacity (type one) according to CT data.
Conclusion. The sensitivity of ultrasound to detect lung changes in COVID-19 is more than 90%. Lung ultrasound has some limitations: inability to determine the prevalence of the process clearly and identify centrally located areas of changes in the lung tissue.
Aim. To explore the effectiveness of corticosteroids in patients with lung damage caused by SARS-CoV-2.
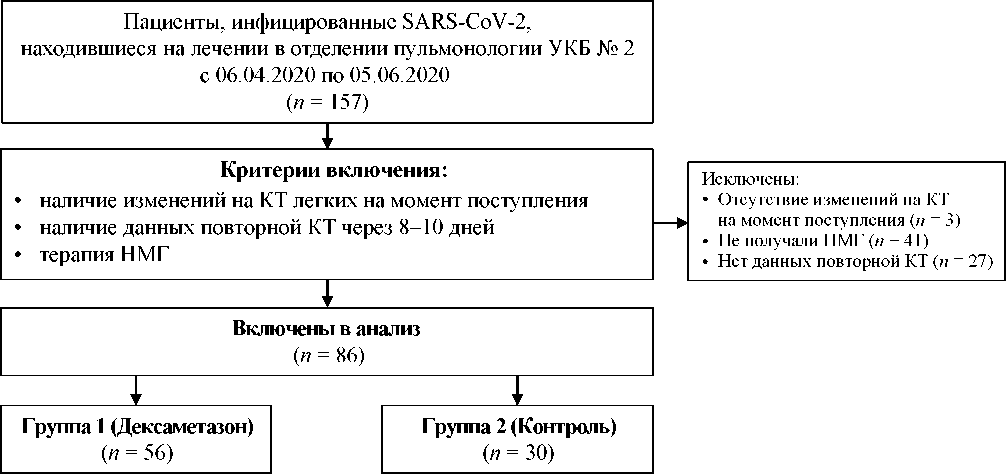
Materials and methods. The retrospective study included patients with confirmed SARS-CoV-2 infection and lung damage diagnosed by computed tomography (CT), who was receiving low molecular weight heparin (LMWH). 56 patients included in Group 1 received dexamethasone 4–12 mg/day for 8–10 days after admission to the hospital. 30 patients included in Group 2 (control group) had no dexamethasone treatment. The laboratory and instrumental data obtained from the patients under admission and for the 8–10th day of the treatment were analyzed. Hospital mortality was evaluated by Kaplan — Meier method. To predict a lethal outcome, we have used the logistic regression method.
Results. By the 8–10th day of hospitalization, only in the Group 1, there was a statistically significant decrease in the volume of lung tissue lesions by CT (p = 0.027), fibrinogen concentration (p = 0.001). A statistically significant decrease of the C-reactive protein concentration was noted for the both groups. Oxygen therapy was more often needed in Group 2 (26 patients — 87%) in opposite to Group 1 (36 patients — 64%) (p = 0.028). Hospital mortality was 3.6% in Group 1 and 13.3% in Group 2 (p = 0.177). There was a trend towards an increase in patient survival in Group 1 between 18 and 28 days of hospitalization (Mantel — Cox test, p = 0.095). Age (p = 0.012), percentage of CT lesions at the time of admission (p = 0.020) and assignment to the dexamethasone group (p = 0.080) were included in the logistic regression equation.
Conclusion. For the patients with SARS-CoV-2 lung damage, treatment with dexamethasone 4–12 mg, started from the first day of hospitalization additionally to LMWH, contributes to positive CT dynamics on the 8–10th day and decreases hospital mortality.
Hydroxychloroquine (HCH) is included in guidelines for treatment of novel coronavirus infection (COVID-19). Data on increased risk of cardiovascular complications when using it have been published.
Aim. To evaluate the safety and tolerability of HCH and azithromycine (AZM) combination for the treatment of the patients with COVID-19 in recommended by Russian Ministry of Health doses in real practice.
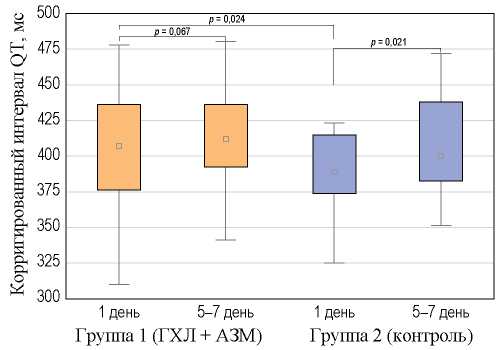
Methods. 132 patients (62 men and 70 women of average age 59.2 ± 9.3 years), 59% of whom had cardiovascular comorbidities, were included in prospective сohort study. 112 patients took HCH + AZM (group 1) and 20 patients took other medications without potential cardiotoxicity (group 2). At the admission to the hospital and after 5–7 days of the treatment corrected QT interval was calculated, new rhythm and conduction disorders, other side effects and hospital mortality have been registering. Relative risk (RR) and 95% confidence interval (CI) were calculated.
Results. Elongation of corrected QT-interval within the normal range was registered in 22.3% of patients in group 1 and in 15% — in group 2. An increase in the QT length to the upper limit of the norm (480 msec) was observed in 1.8% of patients in group 1. There were no statistically significant differences between the groups in the number of patients with prolonged QT interval (RR = 1.488, 95% CI: 0.496–4.466, р = 0.478). The occurrence of new arrhythmias, conduction disturbances and allergic reactions was not recorded. Tolerability of combination HCH + AZM was satisfactory in the majority of patients. The hospital mortality in group 1 was 1.8%, in group 2 — 5% without statistically significant difference (p = 0.374).
Conclusion. A combination of HCL + AZM according to the scheme recommended by the Ministry of Health of the Russian Federation for the treatment of the patients with COVID-19 and cardiovascular comorbidity in inpatient conditions is safe.
In order to enter cells, SARS-CoV-2 virus uses the angiotensin-converting enzyme 2 receptor that is also expressed in retina.
Aim. Determination of the frequency and nature of retinal changes, evaluation of visual functions in patients who have got over COVID-19.
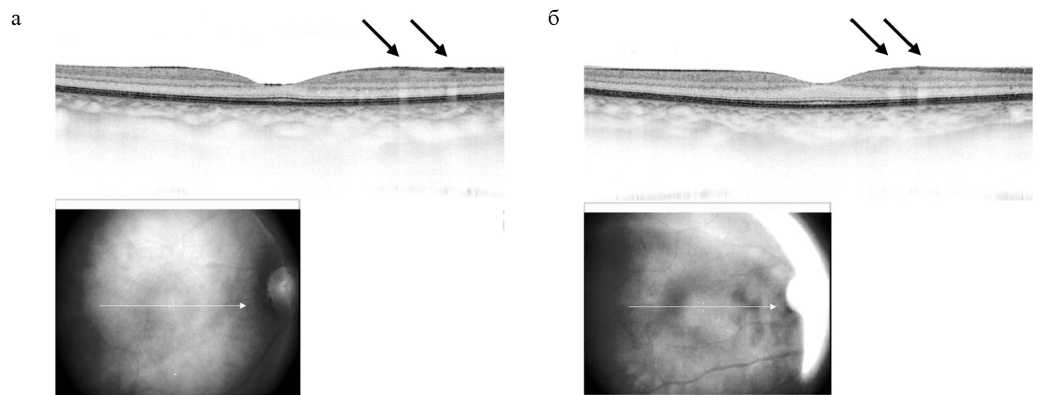
Materials and methods. This observational research includes 31 patients aged from 28 to 79 that got over COVID-19 (with severity according to computed tomography (CT): 1–3) in the period from 15 to 40 days before the research. Standard ophthalmological examination and optical coherence tomography (OCT) were performed; visual acuity measurement and threshold static perimetry were used to assess visual functions.
Results. Pathology of the ocular surface wasn’t detected. Ophthalmoscopy revealed retinal changes in only one patient. At OCT, 27 (87%) patients proved to have de novo changes in the retinal neuroepithelium at the level of the internal plexiform layer and the retinal ganglion cell layer in the form of hyper-reflective polymorphic foci with clear borders; 18 (67%) patients had monocular lesions. The maximum corrected visual acuity didn’t differ from the previously defined one; no violations of retinal light sensitivity were detected. No association was found between the severity of CT lung changes and retinal changes. The detected retinal changes weren’t associated with symptoms of anosmia (hyposmia) and ageusia. OCT repeated after 12–15 days showed no dynamics of hyperreflective foci: they remained unchanged in their shape, echogenicity and size.
Conclusion. De novo changes in retinal neuroepithelium at the level of the inner plexiform layer and the retinal ganglion cell layer were detected according to OCT data in 87% of patients who had undergone COVID-19. Anatomical changes in the retina weren’t manifested by functional visual disturbances. There is no association of retinal changes with lesions of I and IX cranial nerve pairs.
Patients with COVID-19 are typically characterized by severe lung injury with the development of acute respiratory failure. However, in some patients, subjective well-being may remain relatively satisfactory for a long time and, despite severe hypoxemia, they do not complain of shortness of breath.
Case report. We observed a 65-year-old man hospitalized with severe SARS-CoV-2 pneumonia, low level of blood oxygen saturation, but at the same time without complaints of shortness of breath. Only as the disease progressed with a decrease in oxygen saturation when breathing atmospheric air (SpO2 ) lower than 85% he began to notice a feeling of lack of air. The patient’s condition worsened and as a result, he died in the intensive care unit from multiple organ failure.
Discussion. This case clearly illustrates one more feature of the course of pneumonia associated with the novel SARSCoV-2 coronavirus and shows that SpO2 measurement is one of the leading objective criterion that allows a doctor to assess the real severity of a patient’s condition with COVID-19.
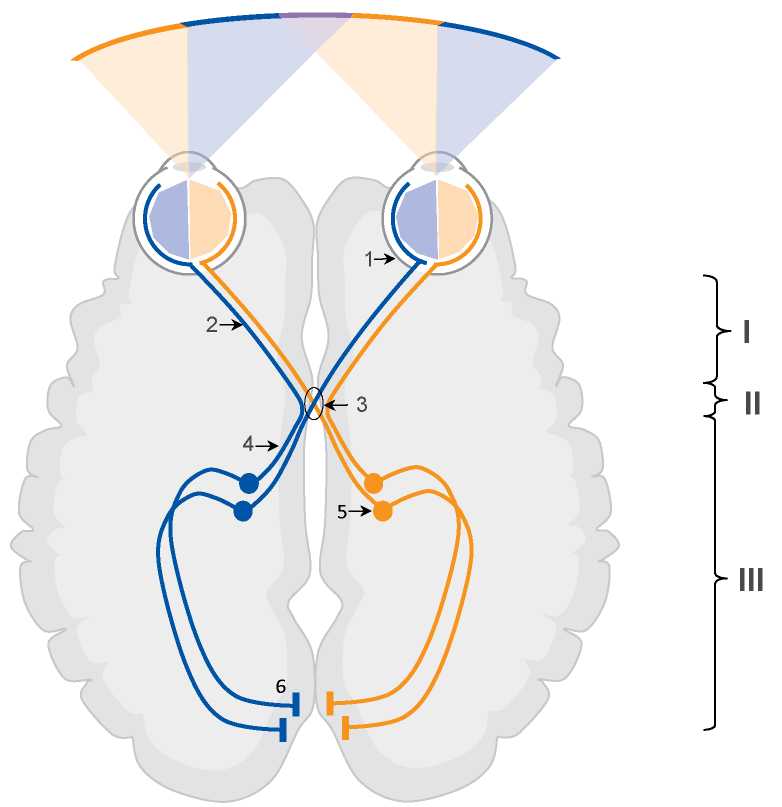
Introduction. Symptoms of lesions of the I, VII and IX pairs of cranial nerves during SARS-CoV-2 infection are observed in about a third of cases. Isolated bitemporal hemianopia as a symptom of optic nerve damage at the chiasmal level in patients with COVID-19 has not been described yet.
Case report. A 65-year-old man with a history of arterial hypertension and myocardial infarction and confirmed COVID-19 infection with severe lung damage on computed tomography. Patient developed bitemporal hemianopia, confirmed by the Donders test, on the second day of hospitalization. CT scan revealed no lesions and organic pathology in the parachiasmatic region and in the substance of the brain. Two days later, there was a complete restoration of lateral vision.
Discussion. The most likely cause of bitemporal hemianopia was microthrombotic or inflammatory lesion at the chiasmal level. Risk factors for thrombotic complications: male gender, age 65, history of cardiovascular diseases, increased D-dimer levels, and signs of systemic inflammation (increased levels of C-reactive protein, fibrinogen, lactate dehydrogenase, and ferritin). An alternative hypothesis for the development of chiasmal syndrome may be direct viral invasion SARS-CoV-2 of the central nervous system.
ISSN 2658-3348 (Online)